Below you will find a growing collection of dietary and health research on type 2 diabetes treatment, with a particular focus on low carbohydrate diets.
Table of Contents[Hide][Show]
Overview
It has long been believed that when people get diagnosed with type 2 diabetes, they’re destined to get progressively worse, take more meds and suffer bad health. That’s simply not the case!
While type 2 diabetes is not reversible from a diagnostic standpoint (once a person has it, they have it), diabetes can be reversible from a physiological standpoint, in many. That is, a person can achieve normal blood sugar levels and metabolic function, and frequently reduce their need for medication. They can live and function like a non-diabetic person.
In addition, people may be able to put their diabetes in remission – defined as HbA1c <6.5% for at least 3 months without glucose-lowering medication.
Research shows this is true (see below) and in our experience with members and subscribers, people are achieving this everyday, even if they’ve had type 2 diabetes for 20 years!
IMPORTANT NOTE: The majority of the research that follows is around type 2 diabetes treatment. It’s important to differentiate ‘reduction of diabetes risk’ from ‘diabetes treatment.’ These are often lumped into the same category but they are two very different concepts. Here at DMP our main focus is on diabetes treatment, along with prediabetes diet and digital lifestyle interventions that get results.
Blood Sugar & A1c
BLOOD SUGAR: Blood sugar is a measure of glucose/ sugar in the blood at any one time. Throughout the day blood sugar can fluctuate in response to numerous factors, mainly food but also exercise, stress, sleep, medications and so forth.
The body is designed to maintain blood sugar levels in a healthy range. It is well established that people with type 2 diabetes and prediabetes should work toward the goal of having normal blood sugar levels because high blood glucose levels causes damage to cells and vessels throughout the body, which can lead to health complications.
Normal blood sugar levels are 70-100 mg/dL or 4-5.6 mmol/L (fasting) and 140 mg/dL or 7.8 mmol/L 2-hours after meals.
While diabetes organizations such as American Diabetes Associations may recommend a higher range (180 mg/dL), research (1,2) shows glycemic values in the normal range are associated with the least risk of complications, if patients can achieve these levels over time.
A1C: A1C is a blood test that provides an average blood sugar measurement for the past 2-3 months. It’s a more accurate measure than blood sugar because it can’t be influenced by meals a person has had today or the day before. A1c is provided as a percentage and the normal range is 4-6%. In some diabetic patients, a higher level of 7-8% may be more realistic. The goal is, where possible, encourage a person to work toward a normal healthy range.
Research has indicated (1,2) that for many people with type 2 diabetes, clinical recommendations for HbA1c levels should be less than 6.5%. HbA1c values in the normal range (less than 6%) are associated with the least risk of complications, if patients can realistically achieve these levels over time.
KEY POINT: Encourage people to achieve glycemic levels in the normal range, if possible, as this shows decreased risk of complications.
Nutrition Therapy and Glycemic Control
Research shows:
- Nutrition therapy has similar or greater effectiveness than medications (3)
- Nutrition therapy can help people with type 2 diabetes reduce A1c levels by up to 2% (3,4).
- Lifestyle intervention provides a 58% risk reduction for diabetes diagnosis in people with prediabetes (4,5).
- While a variety of eating patterns can help treat or prevent, low carb diets are among the most studied eating patterns for type 2 diabetes (3,6).
Type 2 Diabetes Dietary Recommendations
While it is true that there is no one-size-fits-all diet, the ADA Standards of Medical Care in Diabetes: 2022 recommends that to improve health in type 2 diabetes, use strategies common among healthy eating patterns:
“1) emphasise non-starchy vegetables; 2) minimise added sugars and refined grains; and 3) choose whole foods over highly processed foods to the extent possible (p.S50).”
Here at DMP, we have been educating people about nutrient-dense whole food intake since 2015, with emphasis on:
- A high intake of non starchy vegetables
- The inclusion of unprocessed protein sources
- Choosing monounsaturated fat as the predominant dietary fat, but not avoiding nutrient-dense foods that contain polyunsaturated or saturated fats
- A moderate intake of lower carb fruits
- Regular intake of nuts and seeds
- Inclusion of low-fat or full fat dairy products and other whole foods
In addition, a large amount of evidence continues to demonstrates that a lower carb diet is the best dietary pattern for diabetes treatment.
Prior to late 2018, diabetes organizations were very slow to accept low carb diets, however, ADA has for the first time acknowledged it in their 2019 nutrition therapy recommendations that:
- “Low carb eating patterns are among the most studied eating patterns for type 2 diabetes.”
- “Reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia.”
- “For select adults with type 2 diabetes not meeting glycemic targets or where reducing antiglycemic medications is a priority, reducing overall carbohydrate intake with low- or very low-carbohydrate eating plans is a viable approach.”
Likewise, Diabetes Australia released a position statement in August 2018 acknowledging acceptance of a low carb diet as an effective treatment strategy for people with type 2 diabetes.
Now, in the 2022 guidlines, the ADA continues to note that:
“Reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia (p.S63).”
As you will soon see in the research outlined below, the reason for their change of heart is because low carb diets have continuously shown better outcomes for people with type 2 diabetes:
- Decreased blood glucose
- Lower A1C
- Decreased cholesterol
- Increased HDL
- Increased weight loss
- Lower medication need
Our nutrition education has always and continues to focus on a low carbohydrate whole food eating plan that aligns and stays up to date with current scientific research about the most effective diets to treat type 2 diabetes.
Research Links
General Dietary Research References
- Glycemic Targets: Standards of Medical Care in Diabetes—2019: American Diabetes Association. 2019 Jan; 42(Supplement 1): S61-S70. Diabetes Care.
- What’s the ‘right’ range of BGLs? Diabetes Queensland. Published online 13 Nov 2015. Accessed 24 May 2019.
- Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. 2019 May; 42(5): 731-754. Diabetes Care.
- Evert et al. 2013. Nutrition therapy recommendations for the management of adults with diabetes: Position statement. Diabetes Care. 2013;36:3821-3842.
- Diabetes Australia. 2018. Position Statement: Low carbohydrate eating for people with diabetes. Accessed online 2 Sept 2018.
- Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2022 Accessed online 3 Aug 2022.
- Diabetes UK. 2011. Evidence-based nutrition guidelines for the prevention and management of diabetes. Access a copy here.
- Ley SH, et al. Prevention and Management of Type 2 Diabetes: Dietary Components and Nutritional Strategies. Lancet. 2014 Jun 7;383(9933): 1999–2007.
- Sandouk Z, et al. Diabetes with obesity: Is there an ideal diet? Cleveland Clinic Journal of Medicine. 2017;84(1):S4-14.
- Wheeler ML et al. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012 Feb;35(2):434-45.
- Dyson PA, et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med. 2011 Nov;28(11):1282-8.
- Lasa et al. 2014. Comparative effect of two Mediterranean diets versus a low-fat diet on glycaemic control in individuals with type 2 diabetes. Eur J Clin Nutr. 2014 Jul;68(7):767-72.
- Esposito et al. 2009. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med. 2009 Sep 1;151(5):306-14.
- Academy of Nutrition & Dietetics. 2015. Academy Comments re The DGAC Scientific Report [Online]. Available here.
Low Carb Diet and Type 2 Diabetes Research
In 2015, Feinman RD, et al., established a definition of carbohydrates in the diet:
- Very low carb ketogenic diet: 20-50 g per day. Below 10% intake of 2000 calorie diet.
- Low carbohydrate diet: Below 130 g per day. Below 26% total energy intake.
- Moderate carbohydrate diet: 26-45% total energy intake
- High carbohydrate diet (low fat): Above 45% total energy intake
In recent years, there has been an abundance of evidence (see full reference list below) indicating low carb diets lead to greater reductions in A1c levels compared to higher carb diets.
The chart below by Wheatley et al. 2021 shows the outcomes of low carb diets in comparison to other diets.
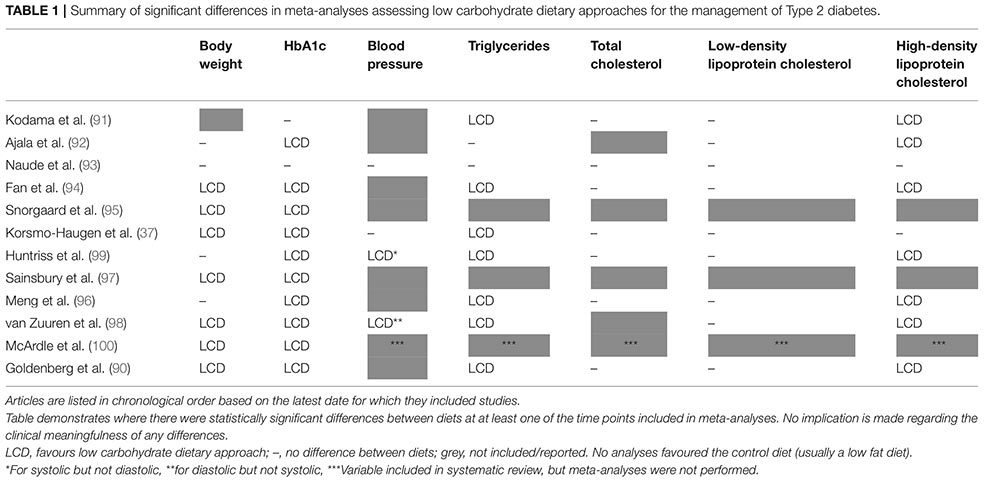
All the items marked LCD have improved on a low carb diet in people with type 2 diabetes – note body weight in the first column.
The grey boxes indicate where the items were not reported in studies. The dash (-) indicates no differences between diet groups.
This is a really great chart to visually show that compared to other diets, a low carbohydrate eating plan improves:
- Body weight
- HbA1c
- Triglycerides
- HDL cholesterol
In the long term (2+ years) other diets have also faired well in terms of A1c reduction. However, consistently low carb diet studies report a reduced need for medication and reduction in glycemic variability, which indicates better overall metabolic function and glycemic control.
CLICK HERE to view a table summarizing research on low carb vs low fat and higher carbohydrate diets.
You can also find links below to various studies about dietary carbohydrates.
Research Links
Low Carb vs Low Fat Research References
- Goldenberg JZ, et al: Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: Systematic review and meta-analysis of published and unpublished randomized trial data. BMJ, 2021. 372: p. m4743
- Huntriss R, et al: The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: A systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr, 2018. 72(3): p. 311-325
- Silverri, et al: Low-carbohydrate diets and type 2 diabetes treatment: A meta-analysis of randomized controlled trials. Acta Diabetol, 2020. 57(11): p. 1375-1382
- Kelly T, et al: Low-carbohydrate diets in the management of obesity and type 2 diabetes: A review from clinicians using the approach in practice. Int J Environ Res Public Health, 2020. 17(7).
- Wheatley SD, et al: Low carbohydrate dietary approaches for people with type 2 diabetes-A narrative review. Front Nutr, 2021
- McArdle PD, et al: Carbohydrate restriction for glycaemic control in type 2 diabetes: A systematic review and meta-analysis. Diabet Med, 2019. 36(3): p. 335-348
- Sainsbury E, et al: Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 2018; 139: pp. 239-252.
- van Zuuren EJ, et al.: Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: a systematic review including GRADE assessments. Am J Clin Nutr 2018; 108: pp. 300-331.
- Snorgaard O, et al: Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 2017; 5: pp. e000354.
- Tay, et al. 2019. Low-carbohydrate diets in type 2 diabetes. Lancet Diabetes & Endocrinology. 2019 May;7(5):331-333.
- Wang LL, et al. The Effect of Low-Carbohydrate Diet on Glycemic Control in Patients with Type 2 Diabetes Mellitus. Nutrients. 2018 Jun; 10(6): 661.
- Samkani A, et al. A carbohydrate-reduced high-protein diet acutely decreases postprandial and diurnal glucose excursions in type 2 diabetes patients. Br J Nutr. 2018 Apr;119(8):910-917
- Saslow LR, et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes. 2017;7(304).
- Myette-Cote E, et al. The effect of a short-term low-carbohydrate, high-fat diet with or without postmeal walks on glycemic control and inflammation in type 2 diabetes: a randomized trial. Am J Physiol Regul Integr Comp Physiol. 2018 Dec 1;315(6):R1210-R1219.
- Sato J, et al. A randomized controlled trial of 130 g/day low-carbohydrate diet in type 2 diabetes with poor glycemic control. Clin Nutr. 2017 Aug;36(4):992-1000.
- Saslow LR, et al. An Online Intervention Comparing a Very Low-Carbohydrate Ketogenic Diet and Lifestyle Recommendations Versus a Plate Method Diet in Overweight Individuals With Type 2 Diabetes: A Randomized Controlled Trial. J Med Internet Res. 2017 Feb; 19(2): e36.
- Tay J, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr. doi: 10.3945/ajcn.115.112581.
- Esposito K, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med. 2009 Sep 1;151(5):306-14.
- Esposito K, et al. The Effects of a Mediterranean Diet on the Need for Diabetes Drugs and Remission of Newly Diagnosed Type 2 Diabetes: Follow-up of a Randomized Trial. Diabetes Care 2014 Jul; 37(7): 1824-1830.
- Yamada Y, et al. A Non-calorie-restricted Low-carbohydrate Diet is Effective as an Alternative Therapy for Patients with Type 2 Diabetes. Intern Med. 2014;53:13-19.
- McKenzie, et al. Should a Low Carbohydrate Diet be Recommended for Diabetes Management?Proceedings of the Nutrition Society. 2017;76 (OCE1):E19.
- Saslow, et al. A Randomized Pilot Trial of a Moderate Carbohydrate Diet Compared to a Very Low Carbohydrate Diet in Overweight or Obese Individuals with Type 2 Diabetes Mellitus or Prediabetes. PLOS ONE. 2014;9(4):e91027.
- von Bibra H, et al. Low-carbohydrate/high-protein diet improves diastolic cardiac function and the metabolic syndrome in overweight-obese patients with type 2 diabetes. IJC Metabolic & Endocrine. 2014;2:11–18.
- Guldbrand H, et al. In type 2 diabetes, randomisation to advice to follow a low-carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Diabetologia. 2012;55:2118–2127.
- Elhayany A, et al. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab. 2010 Mar;12(3):204-9.
- Gannon MC, et al. Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes. 2004 Sep;53(9):2375-82.
- Iqbal N, et al. Effects of a low-intensity intervention that prescribed a low-carbohydrate vs. a low-fat diet in obese, diabetic participants. Obesity (Silver Spring). 2010 Sep;18(9):1733-8.
- Meng Y, et al. Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: A systematic review and meta-analysis of randomized controlled trials. Diabetes Research and Clinical Practice. 2017;171:124-131.
- Hussain TA, et al. Effect of low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes. Nutrition. 2012 Oct;28(10):1016-21.
- Dyson P. Low-carbohydrates diets and type 2 diabetes: what is the latest evidence? Diabetes Ther. 2015 Dec;6(4):411–424.
- Van Wyk HJ et al. A critical review of low-carbohydrate diets in people with type 2 diabetes. Diabet Med. 2016 Feb;33(2):148-57.
- Feinman RD, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015 Jan;31(1):1-13.
- Hamdy O, et al. Fat Versus Carbohydrate-Based Energy-Restricted Diets for Weight Loss in Patients With Type 2 Diabetes. Curr Diab Rep. 2018; 18(12): 128.
- Schwingshackl L, et al. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur J Epidemiol. 2018; 33(2): 157–170.
- Ojo O, et al. The Effect of Dietary Glycaemic Index on Glycaemia in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2018 Mar 19;10(3). pii: E373.
- Saslow LR, et al. Outcomes of a Digitally Delivered Low-Carbohydrate Type 2 Diabetes Self-Management Program: 1-Year Results of a Single-Arm Longitudinal Study. JMIR. 2018;3(3).
Weight Loss & A1C Diets Comparison
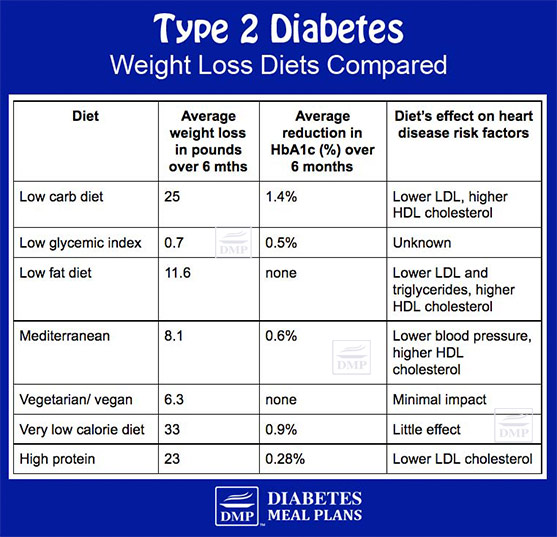
Source: Sandouk Z, et al. Diabetes with obesity: Is there an ideal diet? Cleveland Clinic Journal of Medicine. 2017;84(1):S4-14.
Carbohydrates
The main nutrient that influences blood glucose and insulin is carbohydrates. It is well acknowledged that while the type of carbohydrate is important the amount has the greatest impact upon blood sugar and insulin response.
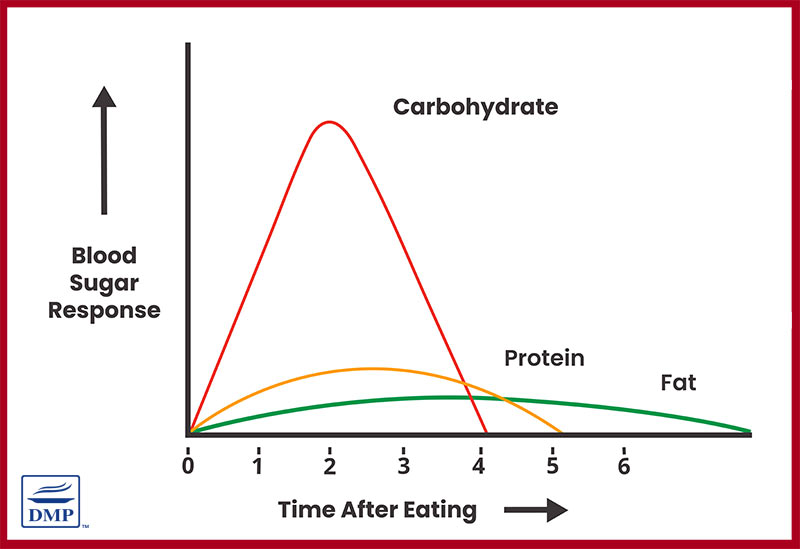
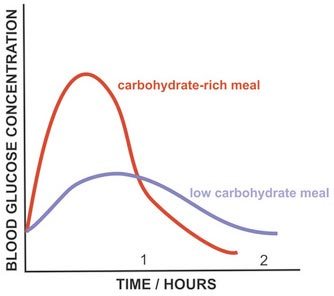
Since this is the case, monitoring carbs/ carb counting remains a key strategy for people to achieve good control. The ADA has only recently (2019) acknowledged that “reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia.”
ADA acknowledge that “studies examining the ideal amount of carbohydrate intake for people with diabetes are inconclusive.”
While that is true, evidence continues to demonstrate that a low carbohydrate approach is an effective way to control diabetes, consistently producing the following results:
- A1c reduction
- Immediate reduction in fasting glucose levels
- Lower medication usage
- Lower risk of hypoglycemia
- Improved cholesterol profile
- Decreased triglycerides and increased HDL
The ADA, Diabetes Australia and Diabetes UK now acknowledge that a low carb dietary pattern can help with diabetes management, a big change since we founded DMP in 2015 when they were all against this dietary pattern.
How Many Carbohydrate Should People Eat?
In 2015, Feinman RD, et al., established a definition of carbohydrates in the diet:
- Very low carb ketogenic diet: 20-50 g per day. Below 10% intake of 2000 calorie diet.
- Low carbohydrate diet: Below 130 g per day. Below 26% total energy intake.
- Moderate carbohydrate diet: 26-45% total energy intake
- High carbohydrate diet (low fat): Above 45% total energy intake
A low carbohydrate diet is considered anything below 130 grams per day, or below 26% of total calories. A low carb diet is not to be confused with a ketogenic diet, which is below 10% of caloric intake. DMP is not a ketogenic website. Both low and very low ketogenic diets improve outcomes in people with type 2 diabetes.
Still, even modest decreases in carbs (20-40% of total calories) can provide benefits for people with type 2 diabetes and prediabetes. The point is, carbohydrate reduction should be encouraged in people with type 2 diabetes.
Low Carb/ Fat/ Protein Ratios
There is no ideal carb, fat, and protein ratio. But let’s calculate two varying amounts of low carbohydrate diets.
In a 1600 calorie diet, the carb/protein/fat ratio of an ideal low carb diet breaks down as follows:
- 10-20% Carbs: 40-80 g/ d
- 20-30% Protein: 80-120 g/d
- 40-60% Fat: 70-110 g/d
Or at a slightly higher carb intake:
- 25% Carbs: 100 g/ d
- 20-30% Protein: 80-120 g/d
- 40-50% Fat: 70-89 g/d
Research Links
Low Carb Diabetes Research References
- Dyson P. Low Carbohydrate Diets and Type 2 Diabetes: What is the Latest Evidence? Diabetes Ther. 2015 Dec; 6(4): 411–424.
- Van Wyk HJ, et al. A critical review of low-carbohydrate diets in people with Type 2 diabetes. Diabet Med. 2016 Feb;33(2):148-57.
- Noakes & Windt. Evidence that supports the prescription of low-carbohydrate high-fat diets: a narrative review. Br J Sports Med. 2016;51:133–139.
- Guldbrand et al. 2012. In type 2 diabetes, randomisation to advice to follow a low-carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Diabetologia. 2012;55:2118–2127.
- Saslow et al. 2014. A randomized pilot trial of a moderate carbohydrate diet compared to a very low carbohydrtae diet in overweight or obese individuals with type 2 diabetes mellitus or prediabetes. Plos One. 2014;9(4):e91027.
- Westman et al. 2008. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutrition & Metabolism. 2008;5:36.
- Naude et al. 2014. Low Carbohydrate versus Isoenergetic Balanced Diets for Reducing Weight and Cardiovascular Risk: A Systematic Review and Meta-Analysis. Plos One. 2014;9(7):e100652.
Fat & Cholesterol
Over the years we’ve all been led to believe that eating fat is bad, so we’ve been pushed toward eating low fat diets. But unfortunately, low fat diets are higher in carbs and sugar, which is not ideal for people with type 2 diabetes/prediabetes.
According to the ADA, “Data on the ideal total dietary fat content for people with diabetes are inconclusive. The type of fats consumed is more important than total amount of fat when looking at metabolic goals and CVD risk. An eating plan emphasizing elements of a Mediterranean-style diet rich in monounsaturated fats may improve glucose metabolism and lower CVD risk and can be an effective alternative to a diet low in total fat but relatively high in carbohydrates.”
While it is agreed that monounsaturated fats provide cardiovascular benefits. As emerging evidence continues to appear, we are learning more about the important role of fat and cholesterol, along with the need to change our perspectives on their intake, including saturated fat intake.
Fat
READ: The definitive guide to fat and diabetes
Research Links
Fats Research References
- Micha R, et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One. 2017 Apr 27;12(4):e0175149.
- Malhotra A, et al. Saturated fat does not clog the arteries: coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventions. Br J Sports Med. 2017;1:1-2.
- Dias CB, et al. Effect of diets rich in either saturated fat or n-6 polyunsaturated fatty acids and supplemented with long-chain n-3 polyunsaturated fatty acids on plasma lipoprotein profiles. Am J Clin Nutr. 2017.
- Hamley S. The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials. Nutrition Journal. 2017;16:30.
- Perona JS. Membrane lipid alterations in the metabolic syndrome and the role of dietary oils. Biochim. Biophys. Acta. (2017).
- Jovanovski E, et al. The effect of alpha-linolenic acid on glycemic control in individuals with type 2 diabetes: A systematic review and meta-analysis of randomized controlled clinical trials. Medicine (Baltimore). 2017 May;96(21):e653
- Yorek MA. Is Fish Oil a Potential Treatment for Diabetic Peripheral Neuropathy? Curr Diabetes Rev. 2017 May 22.
- Errazuriz I, et al. Randomized Controlled Trial of a MUFA or Fiber-Rich Diet on Hepatic Fat in Prediabetes. J Clin Endocrinol Metab. 2017 May 1;102(5):1765-1774.
- Praagman J, et al. The association between dietary saturated fatty acids and ischemic heart disease depends on the type and source of fatty acid in the European Prospective Investigation into Cancer and Nutrition-Netherlands cohort. Am J Clin Nutr. 2016 Feb;103(2):356-65.
- Ruiz-Núñez B, et al. The relation of saturated fatty acids with low-grade inflammation and cardiovascular disease. Journal of Nutritional Biochemistry. 2016;36:1–20.
- Koska J, et al. A human model of dietary saturated fatty acid induced insulin resistance. METABOLISM CLINICAL AND EXPERIMENTAL. 2016;65:1621–1628.
- Paniagua JA. Nutrition, insulin resistance and dysfunctional adipose tissue determine the different components of metabolic syndrome. World J Diabetes. 2016 Nov 15; 7(19):483–514.
- DiNicolantonio JJ, et al. The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease. Prog Cardiovasc Dis. 2016 Mar-Apr; 58(5): 464–472.
- Ginter E & Simko V. New data on harmful effects of trans-fatty acids. Bratisl Lek Listy. 2016;117(5):251-3.
- Imamura F, et al. Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on Glucose-Insulin Homeostasis: A Systematic Review and Meta-analysis of Randomised Controlled Feeding Trials. PLoS Med. 2016 Jul 19;13(7):e1002087.
- Musa-Veloso K, et al. The effects of almond consumption on fasting blood lipid levels: a systematic review and meta-analysis of randomised controlled trials. J Nutr Sci. 2016 Aug 16;5:e34.
- Qian F, et al. Metabolic Effects of Monounsaturated Fatty Acid-Enriched Diets Compared With Carbohydrate or Polyunsaturated Fatty Acid-Enriched Diets in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care. 2016 Aug;39(8):1448-57.
- de Souza RJ, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015; 351: h3978.
- Hooper L, et al. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2015 Jun 10;(6):CD011737.
- Harcombe Z, et al. Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart. 2015; 2(1): e000196.
- Ericson U, et al. Food sources of fat may clarify the inconsistent role of dietary fat intake for incidence of type 2 diabetes. Am J Clin Nutr. 2015.
- Schwab U, et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food & Nutrition Research. 2014;58:25145.
- Viguiliouk E, et al. Effect of tree nuts on glycemic control in diabetes: a systematic review and meta-analysis of randomized controlled dietary trials. PLoS One. 2014 Jul 30;9(7):e103376.
- de Oliveira Otto MC, et al. Dietary intake of saturated fat by food source and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2012 Aug; 96(2):397–404.
- Dilzer A & Park Y. Implication of conjugated linoleic acid (CLA) in human health. Crit Rev Food Sci Nutr. 2012;52(6):488-513.
- Siri-Tarino PW, et al. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010 Mar;91(3):535-46.
- German JB, et al. A reappraisal of the impact of dairy foods and milk fat on cardiovascular disease risk. Eur J Nutr. 2009;48(4):191-203.
- Hartweg J, et al. Potential impact of omega-3 treatment on cardiovascular disease in type 2 diabetes. Curr Opin Lipidol. 2009;20(1):30-38.
- Mozaffarian D, et al. Health effects of trans-fatty acids: experimental and observational evidence. Eur J Clin Nutr. 2009;63:5–21.
- Howard BV, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006 Feb 8;295(6):655-66. Summary: a huge eight year randomized trial that involved 48,835 postmenopausal women aged 50 to 79 years, following a low fat-high carb diet showed zero benefits in reducing heart disease risk factors. The overall conclusion is if you eat a typical Western diet of around 60 percent carbohydrates, your risk of heart disease increases.
Cholesterol
Investigations into the role of cholesterol have gained more attention in recent years.
In 2015, the Dietary Guidelines Assessment Committee (DGAC) released preliminary updates on revisions that were recommended to the American Dietary Guidelines.
Their preliminary statement about cholesterol:
“Cholesterol. Previously, the Dietary Guidelines for Americans recommended that cholesterol intake be limited to no more than 300 mg/day. The 2015 DGAC will not bring forward this recommendation, because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol… Cholesterol is not a nutrient of concern for overconsumption.”
The Academy of Dietetics and Nutrition “supports the DGAC in its decision to drop dietary cholesterol from the nutrients of concern list and recommends it deemphasize saturated fat from nutrients of concern, given the lack of evidence connecting it with cardiovascular disease.”
And as for fat…”The Academy suggests that HHS and USDA support a similar revision deemphasizing saturated fat as a nutrient of concern. It appears that the evidence summarized by the DGAC suggests that the most effective recommendation for the reduction in cardiovascular disease would be a reduction in carbohydrate intake with replacement by polyunsaturated fat.”
Since then an emerging body of evidence continues to indicate that cholesterol in the diet is not a concern. In fact, carbohydrates are more closely associated with higher cholesterol than cholesterol-rich of natural-fat-filled foods. A 2018 study looking at cardiovascular risk factors for 158 countries found that the single biggest risk factor is consumption of carbohydrates. And surprisingly, it’s not just sugar, as we might expect. It’s foods such as cereals, wheat and starchy carbs – all of which are high in carb content.
However, we know that dyslipidemia is common in type 2 diabetes, so what can people expect from a low carb diet?
In most cases, when people switch to a low carb diet:
- Triglycerides go down.
- HDL cholesterol (the “good” stuff) goes up.
- Total cholesterol either goes down or stays the same .
- LDL cholesterol has a tendency to stay the same. However, the LDL particle size often increases (large, fluffy particles), and the LDL particle number goes down (more large particles equals less overall particles).
For those that continue to experience higher cholesterol levels on a low carb diet, there are strategies to manipulate the diet which can help.
READ: Confusions about cholesterol and diabetes resolved
Research Links
Cholesterol Research References
- Richard C, et al. (2017). Impact of Egg Consumption on Cardiovascular Risk Factors in Individuals with Type 2 Diabetes and at Risk for Developing Diabetes: A Systematic Review of Randomized Nutritional Intervention Studies. Can J Diabetes. 2017 Aug;41(4):453-463. Summary: Egg consumption has no impact on cardiovascular risk factors – total cholesterol, LDL cholesterol, triglycerides, fasting glucose, insulin or C-reactive protein.
- Dimarco DM, et al. (2017). Intake of up to 3 Eggs per Day Is Associated with Changes in HDL Function and Increased Plasma Antioxidants in Healthy, Young Adults. — J Nutr. 2017;147:323–9. Summary: Egg consumption improved the function of both LDL and HDL cholesterol but had a predominant effect on enhancing the function of HDL and while on egg per day provided benefits, eating 2 to 3 eggs per day appears to support even greater enhancements in HDL composition and function.
- Fuller NR, et al. (2015). The effect of a high-egg diet on cardiovascular risk factors in people with type 2 diabetes: the Diabetes and Egg (DIABEGG) study-a 3-mo randomized controlled trial. Am J Clin Nutr. 2015 Apr;101(4):705-13. Summary: Consuming 2 eggs per day 6 days per week over a 3 month period has no adverse effects on lipids in people with type 2 diabetes, along with improving hunger and satiety signals. Participants also showed improved intake of monounsaturated and polyunsaturated fat.
- Virtanen JK, et al. (2015). Egg consumption and risk of incident type 2 diabetes in men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr. 2015 May;101(5):1088-96. Summary: In 2232 men, average follow up 19 years, those in the highest compared with the lowest egg intake quartile had a 38% lower risk of type 2 diabetes.
- Fernandez ML. (2012). Rethinking dietary cholesterol. Curr Opin Clin Nutr Metab Care. 2012 Mar;15(2):117-21. Summary: Cholesterol in the diet has very little to do with cholesterol in the bloodstream.
- Gordon T, et al. (1977). High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977 May;62(5):707-14. Summary: Total cholesterol is not associated with risk of coronary heart disease in men and women aged 49-82 years.
- Keys A. (1965). Serum cholesterol response to changes in the diet: II. The effect of cholesterol in the diet. Metabolism. 1965;14(7) 759-765. Summary: A reduction in dietary cholesterol of 50 percent produces only a small effect on blood cholesterol levels.
- Weijers, R. 2012. Lipid composition of cell membranes and it’s relevance in type 2 diabetes mellitus. Current Diabetes Reviews. 2012;8:390-400.
Protein
Protein improves satiety and hunger signals and makes up part of a healthy balanced diet. People with type 2 diabetes and prediabetes should be encouraged to eat healthy protein from lean meats, poultry, game, eggs, nuts, seeds and dairy products.
According to the ADA, “research is inconclusive regarding the ideal amount of dietary protein to optimize either glycemic control or CVD risk. Some research has found successful management of type 2 diabetes with meal plans including slightly higher levels of protein (20–30%), which may contribute to increased satiety.”
There is evidence to suggest that even an intake making up 35% of diets in type 2 diabetes causes no harm.
Additionally, research shows protein may enhance the insulin response to carbohydrates.
Research Links
Research on Protein
- Sucher S, et al. Comparison of the effects of diets high in animal or plant protein on metabolic and cardiovascular markers in type 2 diabetes: A randomized clinical trial. Diabetes Obes Metab. 2017 Jul;19(7):944-952. Summary: Comparing 30% protein from either animal or plant sources in type 2 diabetic patients over 6 weeks. The results showed that consuming 30% animal protein decreased inflammation and uric acid, improved insulin sensitivity and blood glucose control.
- Pederson et al. 2014. High protein weight loss diets in obese subjects with type 2 diabetes mellitus. Nutrition, Metabolism & Cardiovascular Diseases. 2014;24:554e562. Summary: 12 month trial on type 2 diabetics with albuminuria and early renal dysfunction to assess if a 30% protein intake compared to a standard 20% protein diet made any difference to weight loss, renal function (kidneys), or metabolic parameters. The study showed that the higher protein diet had no adverse effects, having comparable outcomes to the standard 20% protein diet.
- Pan Y, et al. Low-protein diet for diabetic nephropathy: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2008 Sep;88(3):660-6. Summary: Low protein diets show no beneficial renal effects in diabetic patients.
- Gannon et al. 2004. Effect of a high-protein, low carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes. 2004;53:2375-2381. Summary: Compared to 15% protein, a 30% protein intake was found to have more positive effects on A1c and insulin, reducing their levels significantly.
We hope you find this research useful in your pursuit to help people with type 2 diabetes and prediabetes gain better outcomes.
If you know of further research that would contribute to our collection, or you have further queries, please contact us.
