Table of Contents[Hide][Show]
In this episode, you’ll uncover the truth behind recent headlines touting a “soups and shakes” diet as a breakthrough for putting type 2 diabetes into remission.
While these claims might seem promising, a closer look reveals a more complex story—one that highlights both the potential and the pitfalls of such a restrictive approach.
LISTEN TO PODCAST
CHAPTERS
2:17 The disproportioned news headlines
3:50 Background on the soups and shakes diet
5:14 Diabetes remission explained
7:21 What is the soups and shakes diet?
9:21 Soups and shakes diet study data dive
13:31 Unsustainable very low calorie diets
16:43 The best way to approach diabetes remission
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
The Hype Around the “Soups and Shakes” Diet
You may have seen sensational headlines like “One-third of type 2 diabetes patients in remission with ‘soups and shakes’ diet” or “Type 2 Diabetes Program Puts 32% Of Patients Into Remission.”
These headlines refer to a new study published in The Lancet Diabetes & Endocrinology, based on the NHS Type 2 Diabetes Path to Remission Programme in the UK.
The program’s focus is on a very low-calorie diet, offering around 800-900 calories per day through soups and shakes over a 12-week period, followed by a gradual reintroduction of regular foods and ongoing coaching.
The study’s results suggest that 32% of participants achieved diabetes remission—a statistic that’s been widely circulated in the media. But before you get too excited, it’s important to understand the full context behind these numbers.
The Reality Behind the Results
Out of the 7,540 people referred to the program, only 1,740 started it, and just 960 completed it.
Of those 960 people, only 450 had two HbA1c measurements recorded, which is crucial for determining whether they achieved remission.
The 32% remission rate is based solely on this small subset of participants—just 145 people.
When you consider the entire group of people referred to the program, the true remission rate is closer to 1.9%. That’s a far cry from the impressive-sounding 32%.
This discrepancy raises an important question: How sustainable and realistic is this diet for the average person with type 2 diabetes?
The Challenges of Very Low-Calorie Diets
One key insight from this study is that while very low-calorie diets can indeed lead to significant short-term results, they are incredibly difficult to maintain. Many participants dropped out of the program, likely due to the extreme nature of the diet.
Descriptions like “brutal,” “grueling,” and “horrendous” are commonly used by those who have attempted such diets. The intense hunger, social isolation, and the mental toll of constant self-denial can make this approach unsustainable for most people.
Moreover, even those who successfully complete the program are advised to continue eating only two-thirds of the food they used to consume. Essentially, this means sticking to a calorie-restricted diet for life—a daunting prospect for anyone.
A More Sustainable Approach: Low Carbohydrate
So, what’s the alternative?
If you’re looking for a more sustainable way to manage or even reverse type 2 diabetes, a low carbohydrate diet, such as the type of nutrition plan we provide here at DMP, offers a proven solution.
Unlike very low-calorie diets, a low carb approach doesn’t require you to starve yourself or live in constant deprivation. Instead, it focuses on reducing your carbohydrate intake to stabilize blood sugar levels and improve insulin sensitivity—key factors in managing diabetes.
Research has consistently shown that low carb diets are effective for achieving diabetes remission, especially when combined with other healthy lifestyle changes.
Unlike the extreme measures of very low-calorie diets, a low carb approach is flexible and can be adapted to your individual needs and preferences. You’ll find it much easier to stick with over the long term, which is crucial for lasting success.
Practical Steps to Get Started
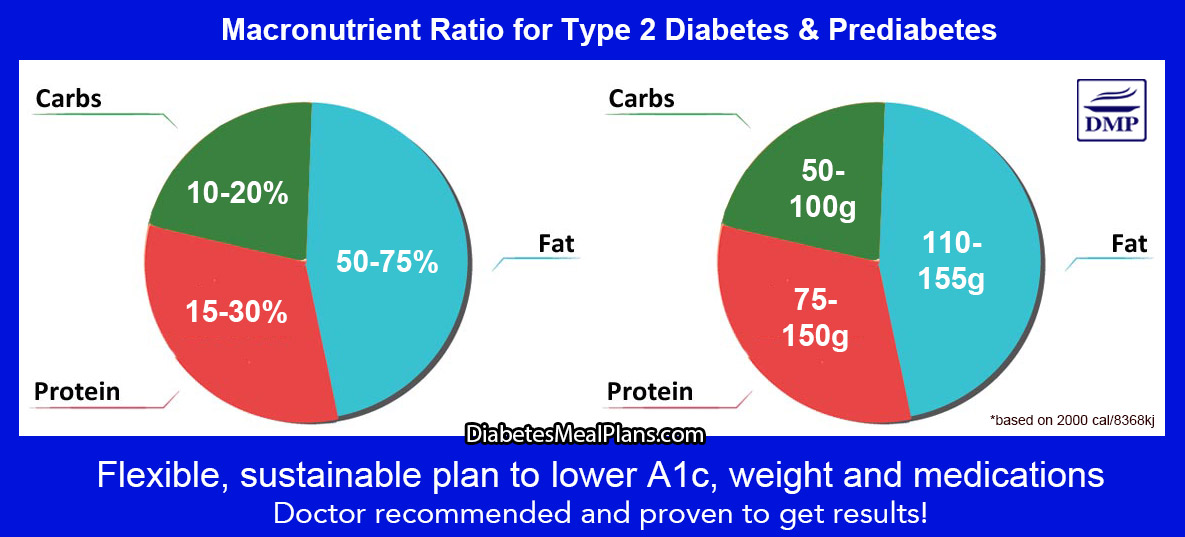
We’re not talking crazy keto or extreme carnivore diets here, but a flexible intake of between 50-100g per day for best results.
If you’re interested in exploring a low carb diet to manage your diabetes, here are some practical steps to get started:
- Download our Food List: Begin by downloading our recommended food list that outlines the best types of foods to eat and avoid. This can serve as your guide for planning meals and making healthier choices.
- Start Gradually: You don’t need to overhaul your entire diet overnight. Start by making small changes, such as swapping out high-carb foods for lower-carb alternatives – the food list will help you get started with that.
- Focus on Whole Foods: Aim to base your diet around whole, unprocessed foods like vegetables, lean proteins, and healthy fats. These foods are naturally lower in carbohydrates and provide essential nutrients.
- Plan Your Meals: Having a meal plan can help you stay on track and avoid the temptation of high-carb snacks and meals. If you want to take the stress out of that and have new inspiring options every week, consider joining us as a member.
Conclusion: Make the Choice That’s Right for You
While the “soups and shakes” diet may sound appealing at first glance, it’s clear that it’s not the most practical or sustainable approach for most people.
Instead, a healthy sustainable low carb nutrition plan offers a flexible, long-term solution that can help you reverse your diabetes without the need for extreme measures.
We know it works because we’ve been supporting our members to achieve fantastic outcomes for over a decade!
Get started today with our recommended food list below, or consider joining us as a member.
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful people and welcome to episode 39. Last week’s episode, number 38, on morning blood sugar levels, otherwise known as fasting blood sugar, was very popular. We explained why morning blood sugar levels are high, as this is often very confusing. And more importantly we covered different methods and strategies that can help you get those high levels back to normal, along with the best natural therapeutic methods as well.
We’ve received a few follow up emails with questions, so if you still have questions about fasting levels, please head over to our website and send us an email or voice message as we may do a follow up Q&A session on this topic – it’s always highly relevant to everyone. And as I said in episode 38, if you try some of those strategies and see changes, be sure to email us to report them, we love hearing about these things.
For today’s episode we’re going to dive into a topic that’s been hot in the media the past week or so, with press releases on Medical Xpress, ScienceAlert, then across women’s health magazines, yahoo news, business sites – you name it, the headlines have been around. If you haven’t seen them yet, perhaps you might as they can take a while to circulate.
You all know my thoughts about the wild west web and I love the headlines, so let me read a few of these to you.
Real-world proof: A third of type 2 diabetes patients in remission with “soups and shakes” diet
The ‘soups and shakes’ diet study shows one third of people with type 2 diabetes enter remission
Doctor says diet of two things for 12 weeks can put diabetes into remission and helps weight loss
Type 2 Diabetes Program Puts 32% Of Patients Into Remission
Okay, we’ve got some interesting claims here, apparently the soup and shake diet put 32% or one third of people with type 2 diabetes into remission.
Is this really true, or just smoke and mirrors? Well…Hold that thought, as we’ll come back to this later.
What these headlines are referring to are some new study results, based on a paper published in The Lancet Diabetes & Endocrinology on August 5th, 2024. The Lancet is a highly prestigious journal so publications there often get lots of media attention. The paper was titled: “Early findings from the NHS Type 2 Diabetes Path to Remission Programme: a prospective evaluation of real-world implementation.” Essentially, the study looked at two-year follow-up data for participants referred to the program provided by the UK National Health Service. We’ll come back to this in a moment, but let’s look at a bit of background for what established this program to be offered by the UK National Health Service in the first place.
This study has come from a background of previous studies that have shown very low calorie diets can achieve remission in people with T2D. The DIRECT and the DROPLET study. Both of those trials were based on the Cambridge Diet, a shake diet that came out of the mid 80s. The Cambridge Diet is now the Cambridge Weight Plan, which interestingly now offers various processed food products in the form of soups, shakes, bars and meals. But we’re not here to talk about that, so back to diabetes remission.
Although there had been documented cases and published reports of remission previously, the DIRECT study was one of the first to bring the concept of diabetes remission to center stage. Simply because they made a whoha about it and described the intervention as the “first evidence from a randomized trial of a dietary and lifestyle intervention with remission of type 2 diabetes as a primary outcome.”
Other people just hadn’t called it remission, other reports called it improving or reversing, or getting off medication, whatever it was, because as we covered in episode 24, which was about remission, the consensus definition term “remission,” wasn’t even decided until 2021, after a 2020 scoping review of studies noted there were 96 definitions of remission. So the consensus of using “remission” as the, shall we say, “proper” term was decided in 2021.
Diabetes remission is defined as an HbA1c of less than 6.5% taking no glucose-lowering medication for at least 3 months.
As we spoke about in episode 24, primarily, there are two ways to achieve diabetes remission. One is through bariatric surgery, the other is through making diet and nutrition changes, with two diets proven to do this, very low calorie diets and low carbohydrate diets.
Coming back to this new paper on soups and shakes diet leading to T2D remission, let’s take a closer look at some of the details of the study, which looked at two-year follow-up data for participants in the program.
Essentially, because of the results of the DIRECT and DROPLET trials, the program was offered in the UK via the National Health Service to implement a similar program in the real world. The actual program is called NHS Type 2 Diabetes Path to Remission programme, but it’s become more well known in the UK as the soups and shakes program or soups and shakes diet for type 2 diabetes. The program goes for 12 months and starts with 3 months of soups and shakes that provide around 800-900 calories per day, along with weekly coaching sessions over the first month and bi-weekly in the two months following. The next 4-6 weeks involved food reintroduction and at least 4 coaching sessions. The remainder of the 12 month duration involved maintenance of goals with at least monthly coaching sessions.
Essentially we’re talking about a very low calorie meal replacement diet, which was offered to people in the real world, not in a clinical trial like the previous studies. But although they’ve said it’s real world it’s not really, because it is still an intervention with lots of coaching and involvement.
So, we see these things in the news all the time and the details are often misreported or over exaggerated or pushed out of proportion. So with many studies we have to look at the details more closely. So I read the paper, and even to me, the way they reported the data was very confusing, and there were errors in the paper too.
There were 7540 people referred to the program over a two year period between 2020 and 2022. 2425 of those people were not interested in taking the program and never attended, another 775 hadn’t started the program by Dec 2022. Only 23% of all people referred to the study had time to undertake and complete the full program by Dec 2022, that’s 1740 people. Out of the 1740 people, only 55% completed the program, that’s only 960 people. The other 45% never completed the program, that’s 780 people. Out of the 960 people who completed the program, only 450 people had two HbA1c measurements recorded, that’s only 6% of the people referred to the study, yet that’s where the news headlines of 32% of remissions was drawn from. If you’re completely confused by this, join the club. I had a difficult time working out exactly how they’d reported this study, as this is a very strange way to report results and I wouldn’t call it robust. What they’ve actually done is bring it right down to the smallest possible denomination.
Basically the study results highlighted across all the news headlines focused only on the 145 people who achieved remission, which would be 32% of the 450 participants who had completed the program AND had completed two HbA1c measurements. That’s only 6% of all the people referred to the program. What about the other 94%? Around 35% were still taking the program and 10% hadn’t started. The other 49% either didn’t take the program in the first place or they didn’t complete it—probably because it is so difficult to follow a very low calorie diet. If all the data were included from the 7540 referred to the program, a large proportion of those still taking or not started would not complete it, that’s the reality. It’s a hard thing to follow.
And if we were to include all the data as it is, there were 7540 people referred to the program over a two year period. That means 52% of people did not complete the study overall. So if we’re looking at it from a real world perspective, then it might be more accurate to say that only 1.9% of people referred to the program during this two year period achieved T2Diabetes remission. If we are looking at it as a real world report of how people were doing after two years of referral to the programme, the reality is, the majority of people didn’t take the program, didn’t complete it or hadn’t completed it and only a very small percentage of people managed to achieve remission. 1.9% of the total number referred to the program, which sounds a lot different to 32%, doesn’t it?
To reemphasize again, very low calorie diets are extremely difficult to follow. And in order to sustain the results, the program recommends people always consume around two-thirds of the total amount of food previously eaten. So basically, you’re stuck on a calorie-restricted diet for the rest of your life.
Back in episode 24 where we covered remission, Helen pointed out that it seems diets like these require extraordinary superhuman self control and denial. And yes, they certainly do. People have personally described these very low calorie diets as brutal, grueling and horrendous, as you can probably imagine. It is not pleasant to experience insatiable hunger, intolerable struggles with internal willpower and self-discipline, inability to socialize – yes, that sounds brutal and horrendous to me too and I would never wish or enforce that upon anyone.
As noted in episode 24, one of the primary issues with very low calorie diets is they cannot be sustained long term, if they can be sustained at all, which is the case for many. They are just too restrictive. And when it comes to reality, if something can’t be sustained long term, then we have to question how effective that strategy really is, because unfortunately, the results you achieved probably won’t be sustainable. Debates also continue about the safety of these diets and their potential to cause harm to the body. And with this new study, concerns from eating disorder charities have been raised about people being put on a diet. That is certainly a concern because if people are offered this type of diet in clinical practice by their doctor, they may think this is the only way to achieve remission or improve their diabetes. For many people, this may trigger disordered eating behaviors, mindset issues, internal struggles, and overall negative outcomes.
As we also noted in episode 24, what also works to achieve diabetes remission is a low carbohydrate diet. We’re not talking crazy keto or extreme carnivore type diets. Yes there is research to show keto diets can be effective for T2D remission too, but there’s one major issue here again – they are unsustainable for most people. As for the carnivore diet, that is literally a fad diet, as there is no clinical research published, as much as people want to spin it this way or that.
Something else that’s interesting about the soup and shake diet is that it is a low carbohydrate plan, with the soups and shakes providing around 121-125g carbs per day. The food introductory phase of the program also includes recipes and meals that are low carbohydrate.
From our perspective to achieve remission, there is no need to go to extremes. What we’re talking about is taking a long term sustainable healthy low carbohydrate approach, which is the type of approach we’ve been encouraging for more than a decade. And it has certainly helped thousands of our members and subscribers completely change their diabetes health and achieve remission too.
A healthy low carb diet is really a very flexible way of eating that is sustainable over the long term. You won’t have to go bury your head under the covers in the bedroom away from the family because you’re starving, tired and irritable.
A healthy low carb eating plan does not require starvation or deprivation, with allowance for a wide variety of foods and meals to enjoy. You can still feel like a real human in any situation. And it’s been proven time and time again in research to be the most powerful and sustainable approach as well. I stand firmly in my recommendation of this, as I have not seen any substantial scientific proof otherwise at this point. And remember, it’s all about evidence over opinion.
While we don’t encourage very low calorie diets, the one positive thing that has come out of all of these low calorie diet studies is that remission has been acknowledged and that diet has been accepted as an option for T2D remission. And the world is starting to wake up and see that T2D is not a condition destined to get worse and worse where people need to go on more and more meds – oops sorry pharmaceutical companies, we’re catching on to the overmedicalization of health conditions such as T2D. Well, perhaps very very slowly because clearly there are still major issues in our system.
The medical care guidelines state that diet and lifestyle should be a firstline treatment strategy at all stages of diabetes, yet we know that doesn’t happen. Prescribing medication is most common. While science has proven that diet and nutrition can indeed be a firstline treatment strategy at all stages of diabetes, and help people achieve normal blood sugar and A1c and reduce and stop meds, we know it’s still not happening. Prescribing medication is most common. But we know if that’s the only type of care people receive, if people only get standard care, they are likely to get worse and need to take more and more medications. Studies have shown this too, including in my own T2Diet Study. Over the 16 week clinical trial, the people taking the T2Diet Program alongside standard care had an average A1c reduction of almost 1%, (0.94) and they dramatically reduced medications, while the control group saw a minimal 0.26% A1c reduction and increased medications. The type of standard care we’re providing in most clinical settings is achieving next to nothing, or leading to a pathway to more medications and potentially diabetes complications. Current ‘best practice’ guidelines are the opposite of ‘best practice.’
Doctors should be offering diet and nutrition as a solution to diabetes, period. As we spoke about, way back in episode 3, diet and nutrition are the most important part of your treatment. The most important part. If you can get your diet and nutrition right, you can completely change your diabetes health.
With the right diet and nutrition, a healthy sustainable low carbohydrate nutrition plan, you can:
- get your blood sugar and HbA1c levels back to normal
- lose weight if you need to
- Reduce your risk of nasty diabetes complications
- reduce or eliminate your need for medication
- Improve cholesterol and blood pressure
- Decrease insulin resistance and improve insulin sensitivity
- Decrease liver fat and normalize liver function
- Decrease pancreatic fat and improve pancreatic function
- Decrease inflammation
- Reduce hunger
- Increase energy
- And even achieve diabetes remission
But, in terms of this soup and shake diet we’ve talked about today. Yes, it may work and if you want to try it, go ahead. But it comes with many downsides. On the other hand, a healthy sustainable low carbohydrate nutrition plan provides many proven benefits and is flexible and sustainable long term. If offered the choice, I know my preference, what about you?
As I said in episode 24 where we covered remission, please don’t get sold a race to remission or buy into any weird or crazy dietary proponents. It’s just not necessary. The key to any permanent change is sustainability!
You can get started today with a sustainable eating approach. If you don’t yet have a copy of our recommended food list, head over to Type2DiabetesTalk.com/foodlist to get a free copy. This food list is the exact same one provided to our members. Make some changes to your eating plan so that it more closely aligns with the food list, as it provides a proven practical nutrition overview for you to achieve better blood sugar and A1c results. The food list also contains some delicious recipes, so I’d recommend you try those too.
Back in episode 33 we covered some diabetes bloopers and Tim said he was told by his doctor that “I wouldn’t have diabetes if I wasn’t fat. Even my Dr told me if I would just lose weight and go down to 150 lbs it would cure the diabetes. She told me to get bariatric surgery to take 80% of my stomach out. I said no thanks. Next time I saw her she said I see you like being fat since you decided to not get the surgery.
Does this sound like a familiar situation to you? If you said yes, you’d be joining many others. The stigmatization of weight is a crucial issue in healthcare. Next week we’re diving in to explore more about it, and sharing a lived experience of Helen and what she has faced in terms of stigma.
Until next week, take care.
Dr Jedha over and out.
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…

Leave a Reply