Insulin is a word that often makes people shudder, especially if you’re diabetic. But, it’s not all bad because insulin is an essential hormone the body needs in order to sustain life. Diabetic or not, we all need it.
Those who aren’t able to make sufficient amounts of insulin, or utilize it efficiently, have the privilege of benefiting from extraordinary scientific advancements this past century, which have paved the way for the manufacturing of exogenous (external to the body) insulin.
The thing is, if you can understand more about how insulin works in your body, and the different types of insulin available to you (should you need to inject), you will feel more empowered to manage your health overall. So let’s dig in and learn more about insulin.
Insulin Metabolism 101
Insulin is the hormone that facilitates uptake of glucose from the bloodstream into the bodies cells – such as cells in your muscles, liver, and so forth.
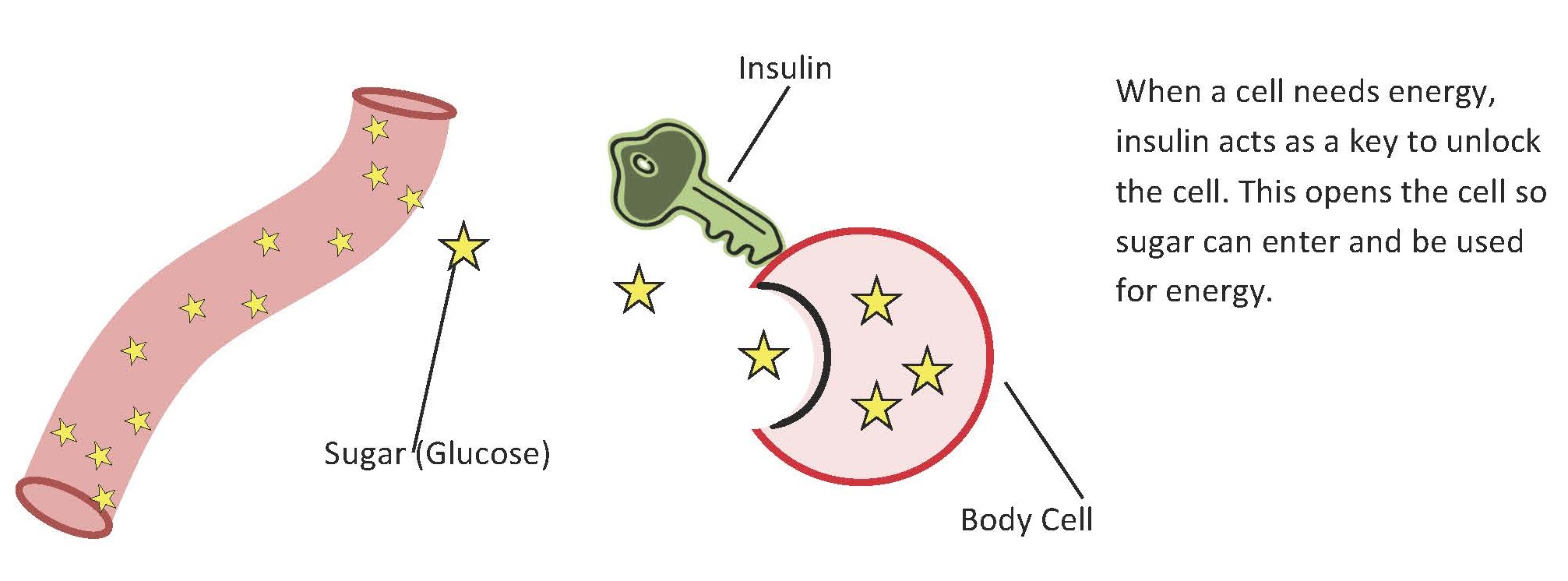
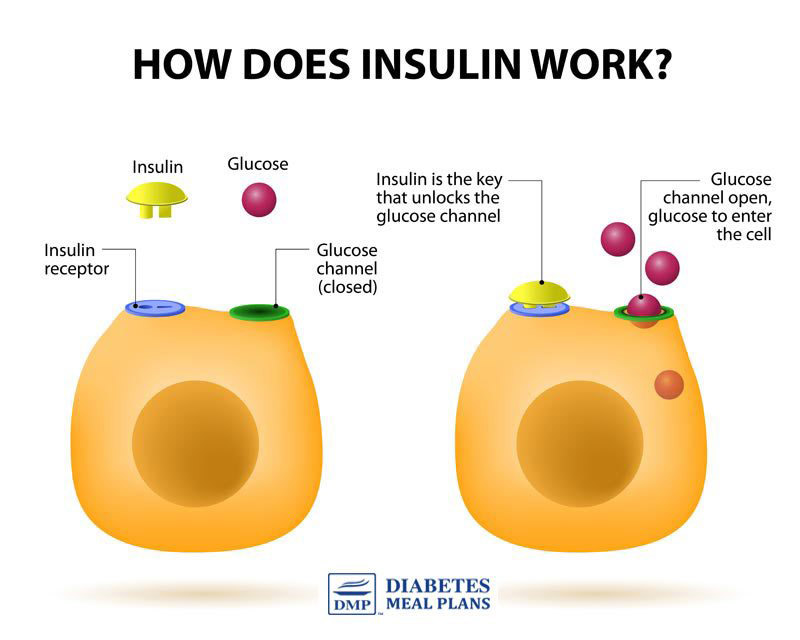
Our body is designed to have an optimal blood sugar range, and insulin is the key that unlocks the cells so that glucose moves out of the bloodstream. Therefore, insulin is the major regulating hormone for maintaining blood glucose at the right levels.
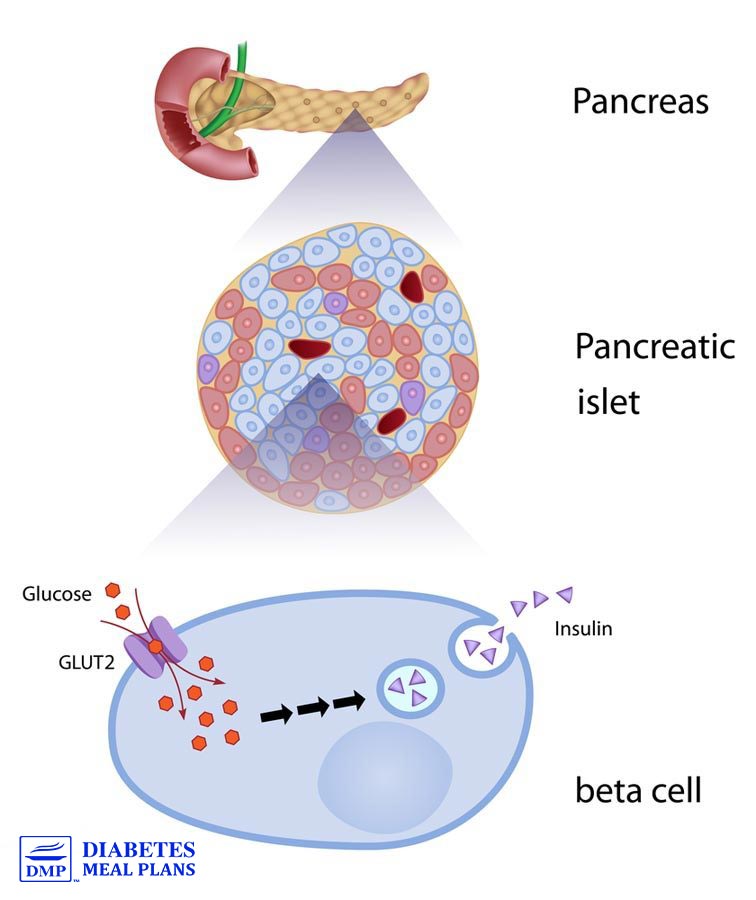
The human body makes ONE type of insulin–called “regular” insulin. It’s produced in the pancreas (specifically by beta cells of the islets of Langerhans) in response to elevating blood glucose levels. Amazingly, the pancreas has a “sensor” that can detect those rising levels, and that’s what stimulates insulin production.
A healthy pancreas will secrete small amounts of insulin throughout the day as needed to compensate for mild glucose elevation. Then at meal times, it secretes a very large amount of insulin as it recognizes the extra glucose (from food…most significantly carbohydrates) is being dumped into the system – meaning, the process of shifting blood sugar is a normal process. Though with diabetes, it becomes abnormal (more on that later).
One analogy that might help you get a better picture of how your pancreas and insulin work, is to think of your pancreas like a thermostat. It’s job is to regulate the “temperature” [glucose levels] to keep the heat just right [glucose levels in a healthy range].
When the thermostat [your pancreas] recognizes it is too cold, the heater [insulin producing cells] is activated and heat floods the home [insulin is released into the body] until it reaches a comfortable temperature [healthy blood glucose level], at which point the thermostat [your pancreas] shuts off [stops putting out insulin].
Make sense?
Here’s another way to look at it: you eat food > blood glucose rises > insulin releases > insulin pushes glucose out of the bloodstream and into cells > blood glucose levels go back to normal > pancreas stops secreting insulin.
Here’s a helpful video that shows the process in animated form.
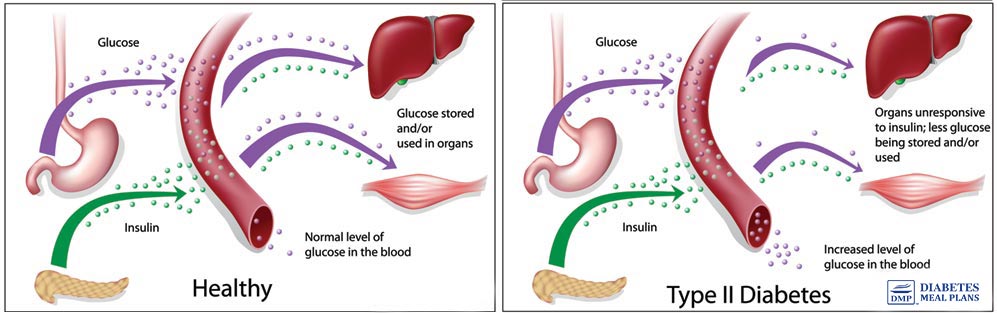
Type 2 Diabetes and Insulin Metabolism
With type 2 diabetes, insulin metabolism is altered.
A person with type 2 diabetes either has a system that:
- Does not accurately recognize elevated glucose [their regulator is ‘off’], OR
- Is not producing enough insulin–what often happens is that poor glucose control causes an INCREASED production of insulin, which causes the beta cells (cells that make insulin) to burn out and die [their heater is rusty and no longer working well], OR
- (Most commonly) Cells become resistant to insulin, otherwise known as insulin resistance – insulin resistance occurs when the insulin receptor cells (the ones that get opened by the insulin key) do not respond to the action of insulin on those cells. The insulin key doesn’t open the cells. The picture below shows a good explanation of this process..
The latter can often be reversed whereas the former two cannot. However, in every case, diet, exercise, and lifestyle are critically important. The difference though is that a person who is unable to produce and utilize sufficient insulin must inject with insulin to maintain control.
The Discovery of Exogenous Insulin – for those that need insulin injections
To replicate the way the body most naturally produces insulin, you would have to give yourself itty bitty shots of miniscule amounts of regular insulin every few minutes, which would be super annoying and not practical. However, this is how an insulin PUMP works and for some diabetics, this can be an excellent option.
Transplanting beta cells has not proven successful and because insulin is broken down easily by stomach acid, it cannot be ingested. For this reason, prior to 1900, sadly most diabetics (most diabetes was type 1 in which people do not produce any insulin) simply died very soon after diagnosis. In 1921, scientists figured out how to isolate insulin from cattle and pigs. This phenomenon saved the lives of thousands of type 1 diabetics, who do not produce any insulin at all. And in more recent decades this insulin discovery has saved the lives of many type 2 diabetics as well (thank you science!).
After many years of studying and sequencing all of the amino acids in human insulin, scientists were able to chemically recreate it through biotechnology, providing a better match and allowing for the potential of unlimited supply (VERY cool!).
Manufactured Insulin
Since pharmaceutical companies are now able to manufacture the properties of insulin, they are also able to alter them, thereby creating different ‘types’ of insulin.
These insulin analogs are differentiated based on their onset of action (how quickly they start working), peak (when it will have its greatest effect), and duration (how long they last).
Rapid Acting:
Names: Lispro (Humalog), Aspart (Novalog), Glulisine (Apidra)
Action: Starts working <15 minutes; Peaks ½ hour-3 hours; Lasts 3-5 hours
Short Acting:
Names: Novolin R or Humulin R (“R” is for “Regular”)
Action: Starts working 30 minutes; Peaks 2-4 hours; Lasts 4-8 hours
Intermediate Acting:
Names: Novolin N or Humulin N (“N” is for “NPH”…don’t even ask!)
Action: Starts working 2-4 hours; Peaks 4-10 hours; Lasts 10-18 hours
Long Acting:
Names: Glargine (Lantus) and Detemir (Levemir)
Action: Starts working 2-6 hours; No peak; Lasts 24 hours
There are also various combinations of the above, but for simplicity sake, we’ll just leave it at this.
Insulin Injections
Remember how the human body only makes ‘regular’ insulin – the equivalent of short acting? Well what’s great about all of these options is that we’re no longer limited to just that short acting kind, which would be impossible to achieve tight control with – especially overnight!.
There are all sorts of insulin regimen options based on the various types of insulin. The most common current regimen we now know achieves the tightest glucose control for most people is called: Basal Bolus.
Basal means baseline. Bolus refers to a single large dose at once. This would involve using a basal (long acting) insulin once daily and bolus (rapid acting) insulin at meal times.
The reason it achieves the tightest control is because it most closely resembles the way the human body naturally produces and secretes insulin – small steady amounts during the day with large bursts at meal times. Often times people starting out on insulin just use basal at first and if meals are consistently low in carbs, a bolus may not be needed. Over time, it may become too difficult to control with bolus alone and they may need to add some rapid or short acting insulin as well.
Keep in mind that cost and coverage can be additional factors for some people as well as number of injections. So while a basal/bolus regimen may be best at achieving tight control, if this is too expensive (or not well covered by insurance) or if a person is unable or unwilling to do 4 injections per day, they may opt to do a 70/30 or 50/50 mix of intermediate and short acting.
Got Questions?
Confused? Overwhelmed? Post your questions below and we will try to help answer them to the best of our ability. Remember, you don’t have to understand this all at once.
Keep reading and researching and having conversations with your healthcare team. Type 2 diabetes is not a simple condition to understand or manage. That’s why we’re here to help you along the way!
Take-Home Tips
The basic take-home points are these:
- Insulin lowers your blood sugar and meals RAISE your blood sugar…to varying degrees depending on what and how much you eat.
- Healthy lifestyle choices such as exercise and healthy diet help the body to use insulin better.
- People who don’t produce enough insulin or are very resistant to the insulin they do produce need to inject themselves with insulin.
- There are many different kinds of manufactured insulin and many different regimens that take into consideration many factors that are important to you.
- Researching, asking questions, and having a positive attitude are key to successfully navigating this maze!
Please share, pin, or tweet this post. :)

Terry Tuytschaevers
I sometimes (more often than I would like) have low blood sugar in the morning just before I wake. Does that mean my Pancreas is producing enough insulin but my body is not able to regulate it appropriately? I take degultide every morning after eating breakfast and Novolog during the day if BS gets too high. Low BS in the early hours of the day (probably in the 4-6 AM hours) is very disorienting. I usually take a snack just before bedtime and this seems to help but doesn’t eliminate low BS intirely. Thanks for your reply.
Malorie: Dietitian (MS, RD, CLT)
Hi Terry,
What is considered “too high”? I just ask as this may be a medication issue depending on how much and how often you end up taking insulin. Other factors that may contribute to hypoglycemia are not eating enough, skipping meals, increased exercise, and drinking alcohol.