Two things we often talk about here at DMP are carbohydrates and inflammation.
Both carbs and inflammation are intimately linked to type 2 diabetes and prediabetes, and your overall health.
For example, we know carbohydrates are the nutrient that most impact blood sugar levels. Hence if you want to lower blood sugar then you need to lower your carb intake.
We also know uncontrolled diabetes leads to higher levels of inflammation, and you may (or may not) be aware that inflammation is responsible for causing some of the complications associated with diabetes.
Today we are going to explore the direct connection between carbs and inflammation in type 2 diabetes and prediabetes.
What Are Carbs?
Carbohydrates are one of three macronutrients your body needs to function. The other two macronutrients are fats and protein. Carbs are made up of sugar and starch molecules such as glucose and lactose.
As you may already know, carbohydrates include foods like:
- pasta
- potatoes
- bread
- corn
- most dairy products
- nuts
- seeds
- fruits
- vegetables
- beans and legumes
- and many other foods
Carbs can be classified as either “simple carbohydrates” or “complex carbohydrates.” Simple carbs digest more quickly and this results in a more rapid increase in your blood sugar, as is the case for simple carbs like white bread or candy.
Complex Carbs
Complex carbs typically contain more fiber, and therefore digestion is slower. Whole grains are considered complex carbs, as are vegetables and nuts. These are often labeled as “healthy carbs.”
Whole grains, along with other “healthy grains” like brown rice or oatmeal are always an interesting debate because there is some research that suggests consuming whole grains may help to reduce inflammation, yet other research suggests whole grains actually contribute to the inflammation cycle
Dietary fiber may, in part, account for the positive observations of whole grains in research studies. Whole grains also have a higher nutrient profile, making them slightly better than their refined counterparts.
After many years of reviewing research, we at DMP agree with the latter school of thought: all grains, regardless if they are refined grains or whole grains, contain a substantial amount of carbohydrate and all carbs will digest (breakdown) into sugar.
Hence, limiting carbohydrates will decrease the amount of sugar in your blood and effectively improve your blood sugar and A1c. As a consequence, inflammation becomes lower and your overall health improves even more.
What Is Inflammation?
Inflammation is your body’s security system. Inflammation tells your body something isn’t right.
If you get a cut on your hand, it’s normal for the cut to become red and inflamed. This is your body’s way of triggering your immune system to help you heal.
Inflammation can also occur on a cellular level, meaning you don’t see it but it’s affecting all your body’s cells. If you develop a virus, inflammation within your cells will follow as a way to notify your immune system to fight the virus.
Inflammation can be measured through blood tests to check levels of common inflammatory markers such as C-Reactive Protein or Tumor Necrosis Factor.
Long term inflammation, often referred to as chronic inflammation, is problematic because your body becomes a bit confused. Normally, inflammation means something is wrong, but chronic inflammation makes your body thinks something is always “wrong.”
This puts high stress on the cells and tissues within your body and it causes them to start to change over time and can result in high blood pressure, high cholesterol, increased weight gain, aches and pains.
But remember, it’s a bit of a vicious cycle. These symptoms are a result of inflammation, but they also cause more inflammation because you’re body recognizes something is wrong but just doesn’t quite know what to do about it.
The bottom line is that inflammation is a necessary bodily response, but left unchecked, inflammation can wreak havoc on your health.
The Connection Between Carbs and Inflammation
Diabetes, and particularly high blood sugar levels, increases inflammation and causes elevated levels of inflammatory markers.
Scientists propose this is due to an increased production in reactive oxygen species (free radicals) and advanced glycation endproducts. Reactive oxygen species (ROS) and Advanced Glycation Endproducts (AGEs) are molecules that cause oxidation (inflammation) in your cells.
More sugar in your blood equates to more sugar (glucose) metabolism, which ultimately results in increased production of ROS and AGEs. Both of which promote cellular dysfunction, consequently promoting more rapid aging and the onset of disease.
Interestingly, fat cells are infamously known for producing inflammatory markers as well, so those who have high blood sugar and are overweight are getting a double whammy.
In addition to high blood sugar and fat cells, other factors that increase inflammation include:
- environmental factors such as pollution and cigarette smoke
- presence of other diseases such as cancer or arthritis
- lifestyle factors like high stress levels
- the quality of your overall diet
You can see how easy it is to be living in a state of chronic, low-grade inflammation… but the good news is that there is something you can do about it.
Please pin, tweet or share; then keep reading.
Research on Diet and Inflammation
Glycemic index (GI) is a measure of how quickly a particular food raises your blood sugar. A food is considered “low GI” if it’s GI value is less than 55. In general, lower GI foods result in less of a blood sugar rise.
While there are mixed results from studies, overall there is a connection between glycemic index and inflammation.
An observational study including 2,735 participants determined that women who consumed a high GI diet were 2.9 times more likely to die of an inflammatory related disease (heart disease or diabetes) compared to women consuming a low GI diet.
While another analysis looking at long term lifestyle changes concluded participants following a low GI diet had lower levels of inflammatory markers and insulin levels compared to those following a higher GI diet.
Does Low GI = Low Carb?
Not necessarily, and this is where it can get a bit confusing. Review the chart below of select foods and their respective GI value and carb count.
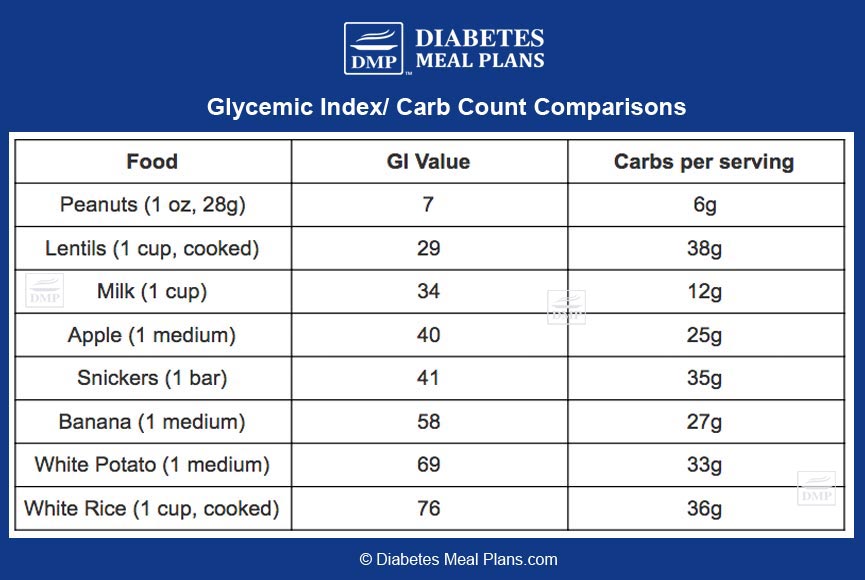
In our opinion, there are a few drawbacks to the glycemic index. Glycemic index measures how quickly a food will raise your blood sugar, but it doesn’t account for total carb content, portion size, or the combination of foods you are eating.
If you solely focus on glycemic index, you may be tricked into thinking that a snickers bar is just as healthy of a choice as an apple – common sense would tell you this is not true!
Relying solely on foods that are low glycemic may be problematic for people with type 2 diabetes and prediabetes because we know that all carbs, regardless of their glycemic index, cause blood sugar spikes. We also know there is a direct relationship between high blood sugar and high levels of inflammation in the body.
In effect, a diet focused on keeping blood sugar levels lower as a whole will be more beneficial in reducing inflammation, rather than a diet based solely on glycemic index.
In fact, one study showed a low carb diet is more effective than a low GI diet for overall diabetes control. After 24 weeks of following a low carb diet 95.2% of participants were able to reduce or eliminate diabetic medication (compared to only 62% of the low GI group.) A 1.5% reduction in A1c was also observed in the low carb group.
Another study comparing 3 diets: a high GI diet, a low GI diet, and a low carb diet, found both a low GI diet and a low carb diet resulted in lower CRP inflammatory markers compared to a high GI diet. Triglyceride and HDL cholesterol levels were more favorable in the low carb diet.
The dietary inflammatory index, which is a tool that measures how “inflammatory” a food is, has been around for sometime now. In every study using the index, researchers have found that the more you stick to a low carb diet, the better off you will be.
And beyond lowering your carb intake, there are a few other well researched nutrients that are known for their anti-inflammatory properties.
Reducing Inflammation with Nutrition
There are certain nutrients available to use that help to capture reactive oxygen species (ROS) and advanced glycation endproducts (AGEs) — we call these nutrients antioxidants.
Antioxidants help make ROS and AGEs less reactive, which is beneficial for your health.
Not coincidentally, most vegetables contain lots of antioxidants and this is just one of the many reasons we encourage you to increase your vegetable intake.
The dietary inflammatory index indicates the top 5 most anti-inflammatory nutrients and foods are:
- Magnesium – seaweed, spinach, chard, sun dried tomatoes.
- Turmeric – a spice that can be eaten both fresh or from the ground spice.
- Beta carotene and vitamin A – carrots, spinach.
- Dietary fiber – from a variety of vegetables, lower carb fruits, nuts and seeds.
- Quercetin – dill, cacao powder, red onions, spring onions.
Conclusion
What you eat every day is very important!
The food you eat on a daily basis can either promote health or disease – the choice is yours everyday.
As a person with type 2 diabetes or prediabetes, first and foremost you need to lower your blood sugar and A1c levels. This will prevent the production of ROS and AGEs, and help reduce unnecessary inflammation.
Remember, all carbs, regardless if they tout a low GI value or not will digest into sugars. We definitely encourage you to pick low GI foods. BUT as someone who is diabetic/ prediabetic you also need to pay attention to blood sugar levels because we know there is a direct tie to blood sugar levels and inflammation.
Secondly, make sure you are consuming plenty of nutrient rich foods. In particular vegetables, nuts, seeds, meats, fish and poultry, and dairy products. Your body needs the nutrients in these foods to help combat some of the other causes of inflammation.
Need help with your diet and reducing/controlling blood sugar and inflammation?

Laura
I have been off the 21 day challenge. For a week or so.. I need to tell you that I am doing much better. My fasting blood sugar level is dow to 7.7. Which is great for me being down from 9.4+-. I am still losing weight slowly. Thankyou for your support. I would love to join as a member but I live in SA and our monetary value is bad. And yes as a pensioner we have very little to live on. I am happy to be part of your programmes.
Emily - Dietitian (MS, RD)
That is fantastic progress, Laura. Keep up with the small changes and you will continue to see big results.
mary
this sounds interesting, but when you have fatty liver disease, isnt eating meat or fat going to not help with fatty liver. so much info out there, so what is right and wrong.
Emily - Dietitian (MS, RD)
We know nutrition information can get confusing, and it doesn’t help that there is so much misinformation floating around out there. Our mission is to provide you with the most up-to-date, research backed evidence in an easy to understand way. :)
Rest assured that fatty liver is most commonly associated with obesity and uncontrolled diabetes (NOT fat in your diet.) Therefore actually eating more meat and healthy fat, plus plenty of vegetables is going to be your best defense against fatty liver. You can read more about fatty liver in this article.