If you have diabetes, you may be curious about the signs and symptoms of kidney disease?
What tests will your doctor run if they suspect kidney disease? And what treatment options are out there?
Keep reading, as we’ll answer these questions and more about kidney disease and type 2 diabetes.
What Are The Kidneys and What Is Their Role?
We’re born with two kidneys. They are bean-shaped organs that sit opposite each other on both sides of the body at the lower of the back, against the back muscles.
The kidneys work to remove waste products and excess fluid from our bodies.
Each kidney is made of up nephrons that contain a glomerulus and a tubule. These filtering units are filled with tiny blood vessels.
Blood enters the glomerulus and is filtered and the fluid passes into the tubule where chemicals and water are added or removed based on what our bodies need at that time. Things that are not useful are excreted as urine.
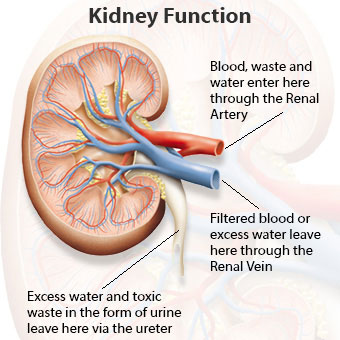
Protein and red blood cells are too big to pass through the blood vessels so those are kept.
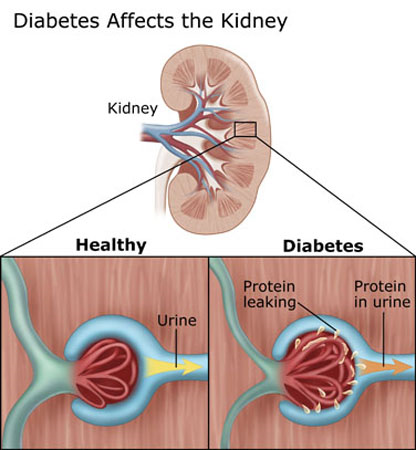
When blood sugar levels are high it can cause damage to the small blood vessels and after a while they start to “leak” protein into the urine.
An early indicator of diabetic kidney disease is this increase in the amount of albumin (or protein) in the urine called albuminuria.
Not everyone who has diabetes will develop issues with kidney function, but kidney disease is a complication of long-standing, uncontrolled or poorly controlled diabetes.
Other factors that increase your risk for kidney dysfunction include:
- Older age
- High blood pressure
- Family history of kidney disease
- Certain ethnicities such as African American, Asian, Pacific Islander, and American Indian.
- Smoking
- Not being active (sedentary lifestyle)
- History of heart disease
According to the CDC approximately 1 in 3 adults with diabetes may develop chronic kidney disease.
Diagnosis of Kidney Disease
Your doctor may perform a urine test called Albumin to Creatinine Ratio (ACR) to check for protein in your urine. 30mg/g or less is normal, more than that can be a sign of kidney disease.
Blood tests include:
Serum creatinine: Creatinine is a waste product from normal breakdown of muscles in your body. Your kidneys will remove creatinine from your blood, but if they are not functioning properly the levels of creatinine can rise in your blood.
Creatinine levels >1.2mg/dL in women and >1.4mg/dL in men may be an early sign of the kidney disease.
Blood urea nitrogen (BUN): This comes from the breakdown of protein in the food we eat. A normal level is between 7-20mg/dL. This level rises as kidney function decreases.
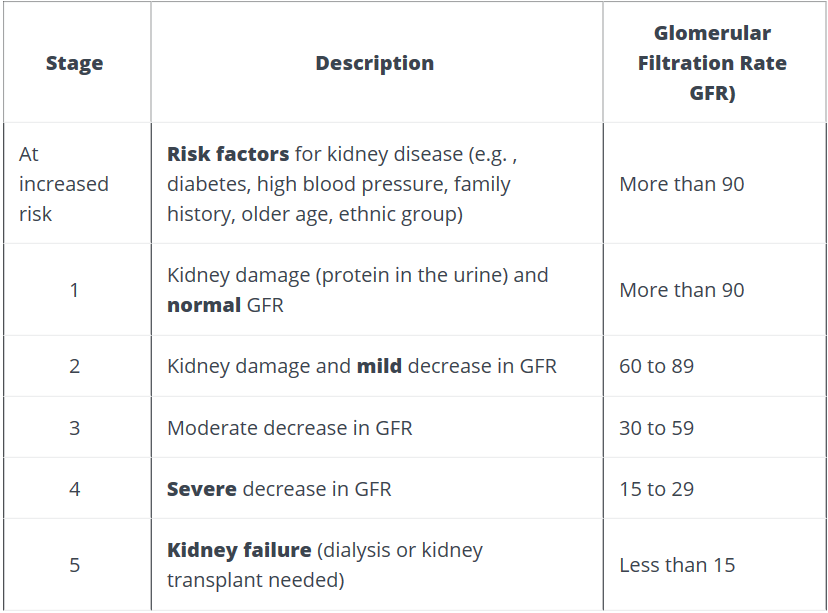
Glomerular Filtration Rate (GFR): This measures how well the kidneys are removing wastes and excess fluid from our blood. Normal values are 90 or greater.
Values between 89-60 can be normal for some depending on age because our GFR tends to decrease as we age.
A level below 60 is a sign that kidneys are not working properly.
Once GFR is below a value of 15, dialysis or a kidney transplant is required.
Your doctor may also perform certain imaging tests such as an ultrasound to review your kidneys’ structure and size.
Staging of Kidney Disease
Effect of Kidney Problems on the Body
One of the first symptoms of kidney problems that you might see is fluid buildup such as ankle swelling, which can lead to weight gain.
Other symptoms include:
- decrease in sleep
- decrease appetite and concentration
- upset stomach and vomiting
- weakness and fatigue
- itching
- muscle cramps
Our kidneys produce hormones that are involved in producing red blood cells, so aneamia is also associated with kidney disease.
As kidney function continues to decline, other health issues can arise:
- low calcium and high phosphorus levels, which can cause issues with bones
- high potassium levels in the blood that can cause high BP, swelling in legs, shortness of breath
- infections
- weakened immune system
- depression
The kidneys also play a role in the breaking down and clearing of insulin from the body. So, insulin will stay in your body longer, which may require less insulin as kidney disease progresses. This can also put you at risk for a low blood sugar or hypoglycemia.
Treatment and Management of Kidney Disease
Keeping your blood sugar and blood pressure at goal levels is the best way to prevent or slow the progression of diabetes-related kidney disease.
Your kidneys help to remove excess potassium and phosphorus from your blood, so as kidney disease progresses into the later stages you may have to limit certain foods that are high in potassium and phosphorus depending on your lab values.
When kidney damage progresses into what is called “end-stage kidney disease”, dialysis or a kidney transplant will be needed.
Your doctor may want to put you on certain medications to help protect kidney function.
Also, there are certain diabetes medications that have been shown to decrease the risk for kidney failure in those with type 2 diabetes and kidney disease.
These include certain SGLT2 inhibitors that have been shown to decrease risk of kidney failure and cardiovascular events as well as prevent and slow the progression of kidney disease in those with type 2 diabetes and kidney disease.
The CREDENCE (2019) trial found that a SGLT2 inhibitor decreased the risk of need for dialysis or transplantation and death from renal or cardiovascular causes by 30%.
Other medications such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs) and GLP1 receptor agonists may also aid in protecting kidney function in those with type 2 diabetes.
Your doctor can discuss more about these options and if certain medications would be right for you.

Leave a Reply