Table of Contents[Hide][Show]
In this episode, you’ll learn about the GLP-1 medications Ozempic and Wegovy, which have gained significant attention for their role in managing type 2 diabetes and aiding in weight loss.
While these medications offer potential benefits, it’s essential to understand their implications and how they fit into a broader strategy for managing your health, especially in the long-term.
LISTEN TO THE PODCAST
CHAPTERS
3:13 What is GLP-14:49 What are Ozempic and Wegovy
10:51 Potential consequences and risk factors of GLP-1 agonist drugs
14:16 Long term efficacy of GLP-1 medications and additional risk factors
20:23 Proposed benefits of GLP-1 drugs21:31 Risks versus benefits
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
The Rise of Ozempic and Wegovy
Ozempic (semaglutide) was initially approved as an anti-diabetic medication, with modest doses starting at 0.25 mg per week.
Its primary function is to stimulate insulin secretion when blood sugar levels are elevated, while also suppressing glucagon, the hormone that raises blood sugar levels and is usually elevated in people with prediabetes and type 2 diabetes.
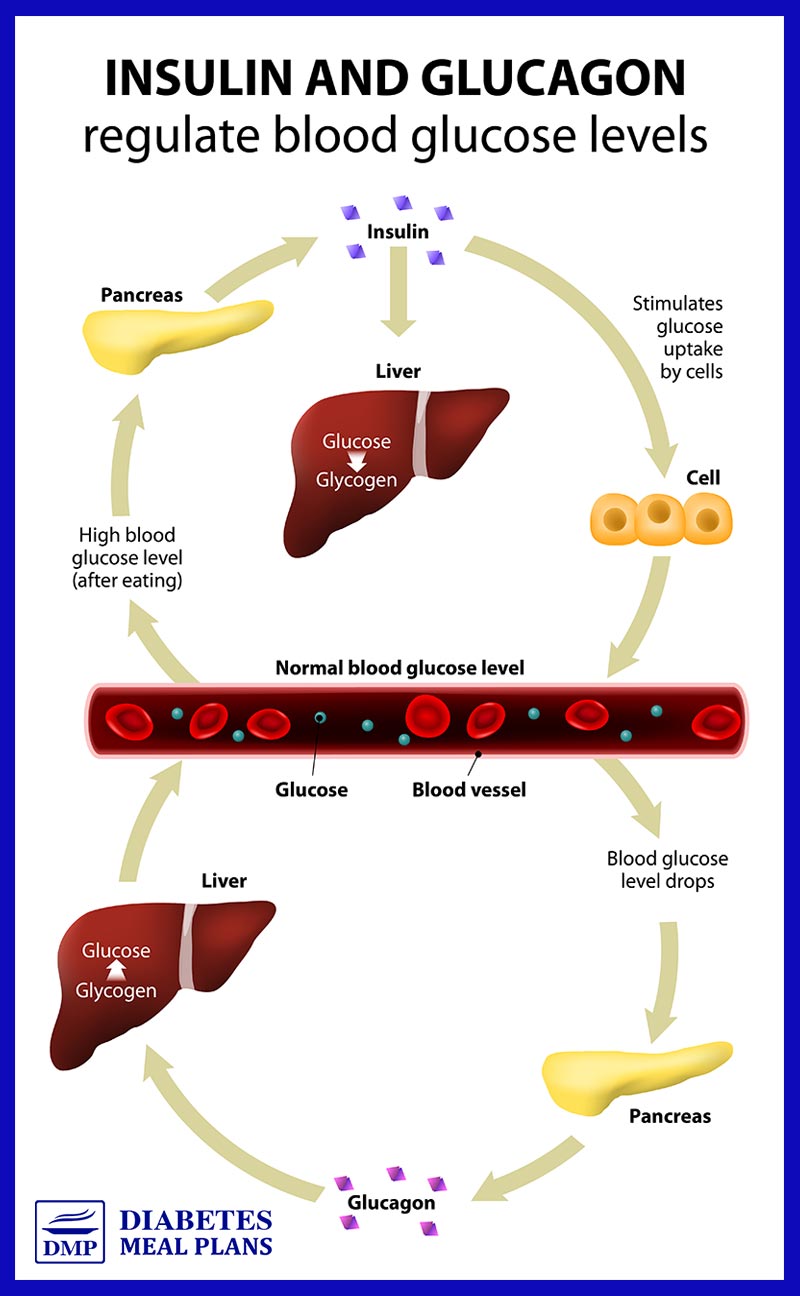
This dual action of GLP-1 helps maintain glucose balance, making it an effective option for people with type 2 diabetes.
As you may know, GLP-1 (Glucagon-Like Peptide-1) is a naturally occurring hormone that plays a crucial role in glucose metabolism. It promotes insulin secretion, delays gastric emptying, and enhances feelings of fullness, which can be beneficial for weight management.
When semaglutide was introduced, it was noted for its appetite-suppressing qualities, leading to unintended weight loss.
Fast forward to today, and Wegovy, essentially the same drug as Ozempic but branded for weight management, has taken the world by storm.
With dosages now reaching up to 2.4 mg weekly (an almost 10-fold increase from the initial 0.25mg dosages!), many people are using these medications in hopes of losing significant amounts of weight.
However, it’s crucial to examine the long-term implications of these increased dosages.
The Impact on A1c Levels
Research shows that even at the original modest dosages, semaglutide can lead to significant reductions in A1c levels.
For instance, studies indicate that participants initially receiving 0.25 mg weekly, then increased to 0.5 mg and 1.0mg, experienced A1c reductions of about 1.5% to 1.8%.
These glucose-lowering benefits have helped many people with their diabetes management.
However, as dosages have increased, it raises questions about the long-term effects and sustainability of using these medications solely for weight loss.
The Impact on Body Weight
In addition to effectively lowering A1c levels, Ozempic and Wegovy have garnered a lot of attention for their significant impact on weight loss.
Clinical trials have shown that these medications can lead to substantial reductions in body weight, making them appealing options for people struggling with obesity or excess weight.
Weight Loss Results
Studies indicate that participants taking semaglutide can lose an average of 5% to 20% of their body weight.
This could translate to a weight loss of up to 46 pounds (about 20 kg) for some individuals, which is a remarkable achievement that many find motivating.
Mechanism of Action for Weight Loss
The weight loss associated with these medications can be attributed to their role as GLP-1 receptor agonists.
By mimicking the action of the naturally occurring GLP-1 hormone, these drugs influence insulin and glucagon and help reduce appetite, increase feelings of fullness, and slow gastric emptying, which contribute to reduced caloric intake.
Sustainability of Weight Loss
While the initial weight loss can be encouraging, it is essential to consider the sustainability of these results.
Research indicates that many people may struggle to maintain their weight loss over the long term, particularly when they discontinue the medication.
And that’s where it gets tricky, as many people can’t continue the medication long-term.
Published reports suggest that around 70% of people may choose to stop taking these medications within two years due to side effects or dissatisfaction with their experience.
When the medication is stopped, people tend to regain the weight they lost, and they may even gain additional weight, leading to a cycle of yo-yo dieting.
Potential for Muscle Loss
Another critical aspect to consider is the composition of the weight lost.
Studies have shown that 20-40% of the weight lost while on these medications may come from lean body mass rather than fat.
Losing muscle mass can have detrimental effects on overall health, particularly as you age. Muscle mass is essential for maintaining strength, mobility, and metabolic health, and its loss can contribute to insulin resistance and other metabolic issues.
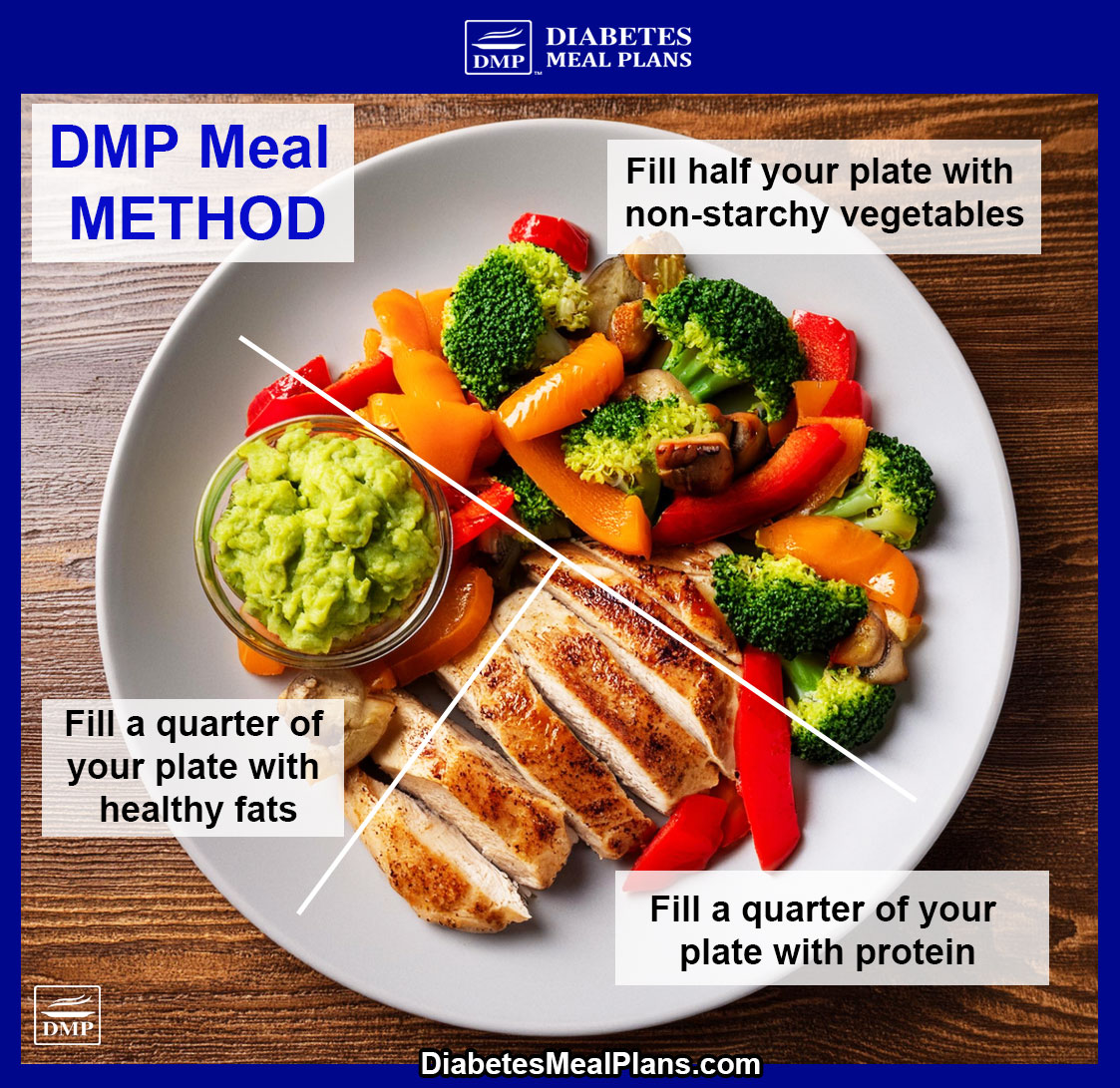
Nutrition Is A Better Long-Term Strategy
While Ozempic and Wegovy can be effective tools for weight loss, they should not be viewed as a standalone solution.
A comprehensive approach that includes nutrition and dietary changes, physical activity, and behavioral modifications is crucial for achieving lasting results.
And in many cases, with the right nutrition support, you can successfully lose the weight without resorting to these drugs!
NEED TO LOSE WEIGHT? Join one of our programs or apply to work one-on-one with Dr Jedha.
Risks of Ozempic and Wegovy
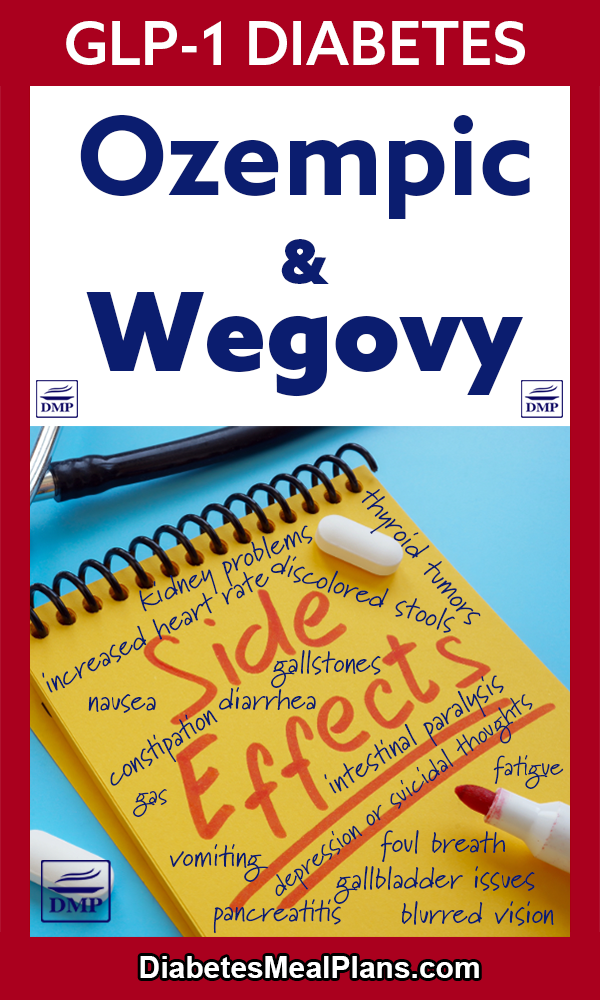
As we discussed in the podcast, while the benefits of Ozempic and Wegovy are touted, there are also serious potential side effects.
Risks listed on the drug websites or among research papers include:
- Thyroid Tumors: Potential risk of thyroid tumors, including thyroid cancer.
- Vision Changes: Possible alterations in vision, including blurred vision and worsening of diabetic retinopathy, with speculation about increased risk of blindness.
- Gastrointestinal Issues: Common side effects include nausea, vomiting, diarrhea, constipation, and abdominal pain.
- Pancreatitis: Inflammation of the pancreas (pancreatitis), which can lead to severe abdominal pain and hospitalization.
- Gallbladder Problems: Increased risk of gallbladder issues, including gallstones that may require surgical removal.
- Kidney Problems: Potential for kidney impairment or failure, particularly in people with pre-existing kidney conditions.
- Allergic Reactions: Serious allergic reactions, including rash, itching, or swelling, particularly of the face, tongue, or throat.
- Increased Heart Rate: Potential for elevated heart rate, which could pose risks for individuals with certain cardiovascular conditions.
- Mental Health Effects: Reports of depression or thoughts of suicide in some individuals taking the medication.
- Ileus: Risk of intestinal paralysis (ileus), which can lead to severe complications and has been associated with numerous fatalities.
From thyroid tumors to changes in vision to gastrointestinal issues and intestinal paralysis, the risks from these medications should be considered carefully.
Practical Steps to Avoid GLP-1 Medications in Type 2 Diabetes and Prediabetes
Focus on Nutrition
While medications like Ozempic and Wegovy can assist in managing diabetes and aiding weight loss, the most effective long-term strategy involves nutrition and dietary changes.
Nutrition and diet are the primary natural treatment strategy for normalizing blood sugar and maintaining metabolic health.
Incorporating whole, nutrient-dense foods into your meals can help improve blood sugar control and support overall health.
Aim to include plenty of non-starchy vegetables, lean proteins, and healthy fats while limiting processed foods and added sugars.
Incorporate Physical Activity
Regular physical activity is crucial for managing blood sugar levels and improving insulin sensitivity.
Aim for at least 150 minutes of moderate aerobic exercise each week, or 30 minutes each day, such as brisk walking, cycling, or swimming.
Strength training is also essential to help maintain muscle mass, to prevent age-related diabetes risk factors.
Monitor Your Blood Sugar
Regularly checking your blood sugar levels can help you understand how your body responds to different foods and activities.
This knowledge empowers you to make informed decisions about your diet and lifestyle.
The Bottom Line
While Ozempic and Wegovy offer promising benefits for managing blood sugar and aiding weight loss, it’s crucial to understand the broader context of your health and the potential long-term implications of taking these drugs.
Medications are just one piece of the puzzle and are best avoided or reduced where possible. Working with your doctor to desprescribe medications is possible.
Focusing on nutrition first is key!
If you need help with getting your health on track and reducing medications naturally, consider joining us as a member. Or apply to work one-on-one with Dr Jedha.
Every single day we’re hearing about our members success in turning their health around. Let us help you too!
“I wanted to see my A1c under 5.7 but my doctor told me that because of the medications I have to take, not to expect that to happen. I got great news today. My A1C is 5.8!! I am so grateful for DMP!”.
~Val
“This way of eating works. Sugar numbers are down and Dr. has taken me off one of my medicines for 3 months to see how I will do.”
~Retha T
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful people, Dr Jedha here and thanks so much for joining me. Today, we’re exploring two medications that have gained significant attention: Ozempic and Wegovy.
It wouldn’t be far-fetched to say that drugs like Ozempic and Wegovy have taken the world by storm. With the promise of losing significant amounts of weight, there has been an explosion of people taking these drugs, to the extent that celebrities and others actually brag about using the medication to achieve their weight loss success, which is just crazy stuff.
Before we dive into this topic I want to note that I’m not sharing this information to scare anyone, for instance, if you might be taking the medications we’re discussing in this episode today. The reason I’m noting this is I know some people can get offended by it. Providing facts from research and the actual product brochures is not designed to scare people, but to responsibly inform people. The evidence is the evidence and it is the truth so if you’re not being informed by your doctor, where else might you be informed about it. It’s important that you have all the information to make informed decisions and choices.
I am always curious to read the research surrounding these drugs and over the past several months have bookmarked several papers that sparked interest. And a few months back I was listening to a fascinating presentation by colleagues who spoke extensively about GLP-1 and these drugs. The information I’m sharing today is the result of combining the research I’ve done, with the things learned from colleagues, along with information directly from the drug websites and product labels.
For our members, you can find all this information and additional information alongside episode 55 in the members library. For others, head to our website for this episode and abbreviated information.
03:13
Let’s start by understanding GLP-1. GLP-1 stands for Glucagon-Like Peptide-1. GLP-1 is a hormone that plays a vital role in glucose metabolism. It is a naturally-occurring hormone produced by our body, in the intestines in response to food intake. One of its primary functions is to stimulate insulin secretion from the pancreas when blood sugar levels are elevated, which helps to lower blood sugar levels.
In addition to promoting insulin secretion, GLP-1 suppresses the secretion of glucagon, another hormone that raises blood sugar levels. Glucagon is elevated in people with pre and T2Diabetes, so this dual action of promoting insulin secretion and suppressing glucagon is crucial for maintaining glucose balance, for maintaining blood sugar balance. Another thing that GLP-1 does is it delays stomach emptying, slowing down digestion, which helps reduce post-meal spikes in blood sugar. It also promotes satiety, or the feeling of fullness, which can be beneficial for reducing cravings and for weight management. Overall, GLP-1 has an impact on both blood sugar control and appetite regulation. And remember, it is a naturally-occurring hormone produced by our body.
04:49
Now, let’s talk about Ozempic and Wegovy. Ozempic and Wegovy – semaglutide – are injectable prescription medications made by the same company Novo Nordisk. These two medications are designed to mimic the effect of GLP-1. Ozempic and Wegovy are known as GLP-1 receptor agonists. They bind to cellular receptors that GLP-1 would bind to, but in a different way, an elevated way. Essentially, they elevate the action of GLP-1 in a way the body couldn’t achieve on its own, amplifying it to certain extremes, depending on dosage. Ozempic and Wegovy are injected medications because taking them in pill form is not effective; the digestive process would break them down, reducing their efficacy. Injecting these medications allows them to enter the bloodstream directly, ensuring optimal absorption and action in the body.
When introduced semaglutide was FDA approved only for use as an anti-diabetic drug. We spoke about this way back in episode 17 and 18, when Su Robotti, a side effects expert came on the podcast as a guest and spoke about her role on the FDA advisory committee when they approved these drugs, it was a very interesting discussion. Point being, Ozempic was first approved only for use as an anti-diabetic drug to lower blood glucose. When the drug was first being used as an anti-diabetic drug, it was noted that the drug had the benefit of reducing appetite and food intake, and facilitating weight loss. Fast forward to now and the drug Wegovy, which is essentially the same drug as Ozempic, just a different brand name, is now approved as a weight loss drug, leading to a wild frenzy that is now occurring across the globe. When Ozempic was being primarily used as an anti-diabetic drug, it was only being prescribed in small modest dosages of the medication, around 0.25mg once a week. For that purpose, these drugs could be warranted where necessary, because at these lower dosages, the benefits of the drug could outweigh potential side effects. However, the surge in popularity for weight loss has prompted an increase in dosages. Currently, Ozempic can be prescribed up to 2.0 mg weekly, while Wegovy has doses that go up to 2.4 mg weekly. This escalation in dosage raises concerns about the long-term implications and potential side effects of higher doses being used for weight loss. Data comparing early prescribed dosages of Ozempic to current practices highlights this significant shift, as initial prescribing was more conservative, focused on managing diabetes, whereas the current trend leans heavily towards weight management at increased doses.
As we covered earlier, these GLP-1 agonist drugs elevate the action of GLP-1 – they suppress glucagon, which helps bring the blood sugar under control. And they also have a direct effect on the fat cells, directly activating fat breakdown. All of that sounds great, right? Anyone wants to bring glucose down and spark fat loss. And in terms of weight loss, it might be easy to get excited about losing 5-20% of your body weight, which is the average range of weight reduction shown in clinical trials. That could amount to up to 46 pounds or 20 kilos, as in some reports – that’s substantial by anyone’s terms. But while the idea of a quick fix may sound appealing, there is much more to consider, as we’ll get to a bit later.
Another key benefit often promoted is that people say they don’t get cravings anymore and that’s because the drug reduces appetite, it suppresses it. Again, anyone of us may think, yes please, I want to reduce the cravings I have that hit me every day at 5PM or 7PM when that sugar monster seems to be calling my name, wanting me to eat that candy or chocolate cake, or crisps or crackers. Later we’ll touch upon why this isn’t a good outcome either.
There was a recent study that looked at what factors influenced the ability of people to achieve a 10% of greater weight reduction when taking semaglutide and these were higher dosages of the drug, persistence with the medication (those who remained on it for a year or more), and patients with a higher BMI being treated. It is very difficult to stay on the medication long term, and therein lies the big issue for several reasons, which we will get to shortly as well.
10:51
Losing weight and reducing cravings and hunger can be powerful motivators for wanting to try the drug. The other side of the equation though, is there are the very real potential consequences, and you do need to take these into consideration. With every medication you take there are side effects to consider. Doctors and pharmaceutical companies may play these down, emphasizing the benefits, but the reality is they could happen to you, they can’t guarantee they won’t.
The most notable concern made by the pharmaceutical company is the possibility of thyroid tumors, including cancer. The rate at which this may occur is still an unknown factor.
Another warning is changes in vision. Studies have shown semaglutide causes changes to vision, including blurred vision, worsening of diabetic retinopathy and macular complications. Data around this side effect is still relatively new, so it’s difficult to conclude how severe symptoms may become, although some studies suggest a potentially higher risk of blindness.
Other possible side effects noted on the product label and clearly on the drug websites, are inflammation of your pancreas (pancreatitis) – we’ve had acute pancreatitis requiring hospitalization, occur in a couple of our members), gallbladder problems (including gallstones that may need surgical removal), kidney problems and kidney failure, serious allergic reactions, increased heart rate, and depression or thoughts of suicide.
These are all pretty serious side effects to consider, should they affect you.
The most common side effects reported by the pharmaceutical company on their website are and I quote, “nausea, diarrhea, vomiting, constipation, stomach (abdomen) pain, headache, tiredness (fatigue), upset stomach, dizziness, feeling bloated, belching, low blood sugar in people with type 2 diabetes, gas, stomach flu, heartburn, and runny nose or sore throat.” Again, a fairly long list.
Certainly we know from the scientific literature that whe most common side effects are gastrointestinal disorders. In fact, studies have reported there are 45 different gastrointestinal side effects, the most common being nausea, diarrhea, vomiting, and abdominal pain, along with others not noted on the product label, such as dry mouth, abnormal gastrointestinal sounds, irregularity in bowel movements, and feces being discolored. Studies have shown that all dosages increase gastrointestinal side effects, which can vary in severity, and range in the length of time people experience them.
14:16
Coming back to the fact that efficacy of the drug relies on a person taking it for at least a year. Many people won’t tolerate the gastrointestinal side effects alone. In fact, we’ve had members hospitalized from dehydration related to suffering the gastrointestinal side effects of semaglutide – these things certainly do happen people, this stuff is not a white elephant that happens on the odd occasion. While it may be possible to achieve a year on the drug, published reports have indicated that within two years of starting the drug, around 70% of people choose to get off the drug because they are feeling incredibly sick on the drug and they don’t want to take it anymore. And that’s a big, big issue.
When you stop taking these drugs, you will gain all the weight back, and likely more. You have to stay on the drug for life in order to maintain the weight loss, and at this early point of the drugs widespread existence we don’t even know if that’s possible or what the longer term effects will be. We also know longer term intake of these drugs is simply not possible for many people, as indicated by the fact that a large majority of people voluntarily want to stop taking the drug within two years.
There’s one other major downfall, research has shown that 20-40% of the weight lost is weight lost from lean mass, which means you’re not losing fat but you’re losing muscle mass. That’s not good, especially as we get older. Muscle mass is essential for maintaining overall health and physical function as it supports mobility, balance, and strength, which are crucial for daily activities. Additionally, having adequate muscle mass contributes to metabolic health by improving insulin sensitivity and aiding in weight management. After age 40, muscle mass can start to decline more noticeably. By age 60, we have an even harder time maintaining muscle and bone mass, and restoring it can be even more difficult, particularly for women with menopause and changes that occur in hormones that affect muscle and bone mass.
Let’s just say you choose to take the drug for weight loss and within a couple of years you decide to stop taking the drug. You will gain back weight and you’ll quickly gain back fat but you won’t gain your lean mass back. That muscle or bone loss can be permanent, if not incredibly difficult to restore. So one of the key downfalls is that on the other side, you will now actually be fatter than before. You might still weigh the same, but you’ll have more fat mass and less lean mass. That’s not good as it can affect strength, mobility, and overall health, not to mention increase insulin resistance and appetite and hunger, likely more than experienced before.
Coming back to those cravings we talked about earlier. Appetite and cravings are dramatically reduced because the drug influences the gut, the intestines, slowing down the movement of the intestines. In response to eating food, our intestines have a natural contraction process that moves everything from our stomach along the intestines for absorption and processing and through to our bowel for excretion. These drugs slow down the natural movement and contraction of the intestines. Food can stay in the digestive system a lot longer than it should. Belching and foul breath can become a problem, as food ferments in the stomach. Something else to consider is that due to the slower intestinal function, digestive function and nutrition absorption can become compromised and this can lead to nutrient deficiency over time.
More than that, it is possible that a complete paralysis of the intestines can occur due to these drugs. This condition is known as ileus and is potentially lethal. Ileus has occurred in people taking these semaglutide drugs and has led to about 20 deaths the last report I saw. But intestinal paralysis has been seen in clinical practice among colleagues, so it is certainly a very real consequence of these drugs. Ileus can potentially lead to permanent paralysis of the intestines, with the need for tubes and bags to handle digestive processes. That does not sound like a fun outcome for anyone, wouldn’t you agree?
Yet another downfall is that although cravings might be reduced initially, this effect wears off around the two year mark, where you will see your cravings and appetite increasing once again, so you need to up the dosage of the drug, which is likely not possible for most as dosages will already be so high.
20:23
What’s interesting is there have been many papers being released about the benefits of these drugs for all sorts of things from improving heart disease, cognitive function to reducing risk of certain cancers, and Alzheimer’s disease. There are a lot of things coming out around this, and so early of the drug being released, it seems rather astonishing.
Certainly, it is true that these reports have examined positive benefits and they sure are hailing these benefits far and wide, no doubt to try to outweigh the negatives. In reality, colleagues have noted that the more likely consequence of these benefits is because the drug is decreasing insulin resistance and improving insulin sensitivity throughout the body’s cells. Insulin resistance is at the center of many chronic health conditions and if we address the insulin resistance, we reduce the risk of heart disease, stroke, Alzheimers, cancer and the list goes on. As we covered in episode 26 on insulin resistance, we can also improve this with nutrition.
21:31
In any case, what we’ve covered here is that the short term benefits may look good, but the long term consequences, based on the evidence, the long term metabolic consequences, do not seem worth the risks.
Is it really possible to keep taking a drug forever? If not, which appears to be the case for many, then you’re not just back at square one, but square minus 10, as you’ll be left with more fat mass and less lean mass, and again, you’ll have to look at other options. You’ll be left to look at options you could have potentially used in the first place – namely, focusing on nutrition.
By far, the healthiest, most sustainable way to lose weight long term is through nutrition and dietary changes, coupled with changing some things in our lifestyle. If you’ve listened to the podcast a while you’ve heard of Wilma’s 79 pound weight loss, that’s 36 kilos. Head to our testimonials page to view hundreds of testimonials from our members with their blood sugar and weight loss success. Carin, losing 15 pounds in a few months, Suan 24 pounds, Lyn 44 pounds, Cheryl 21 pounds, and the list goes on. And most tell us they are so happy with the weight loss because they have tried to lose weight for years and never could. We can help you lose weight, naturally, so please head down to our website and join us as a member. It is difficult to do it on your own. You need the right guidelines, the right tools and the ongoing support to achieve it, that’s what’s helped all our members get better results than they’ve ever had. Just head to our website to view the testimonials and please join us – you don’t have to do it alone!
Again, I want to emphasize that I’ve shared this information today to inform you about potential consequences of these semaglutide medications. If you’re already taking these drugs, you may wish to consider working with your doctor to reduce them over time, in conjunction with working on your nutrition with a program such as the T2Diet Program or joining us as a member. If you’re not yet taking them but have been considering the option, perhaps now you may reconsider the longer term outcomes and pursue a different option, focusing on your nutrition. Either way, I hope you have found this episode informative and helpful.
If you do have further questions or input, head to our website. Comments are always open on our blog where we post these episodes and you can also submit questions via voice message or email.
That’s all for now. Take care of you.
Dr Jedha, over and out.
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…


keto or low carb and jardiance do not mix
Jardiance is an SGLT2 inhibitor medication, which some studies claim causes ketoacidosis. Ketoacidosis is a very rare adverse event, the cause of which is not fully known. However, lowering carbohydrate intake is noted as a caution for people taking SGLT2 inhibitors – though it appears to be more cautionary for people following keto diets. DMP guidelines are not a keto diet.
It is not fully known if lowering carbohydrates causes ketoacidosis, as it is usually present in relation to metabolically stressful events, such as surgery, extensive exercise, heart attack, stroke, severe infections, prolonged fasting, and other stressful physical and medical conditions. Often people stop SGLT-2 inhibitors with both keto and low carb, as they often don’t need them and can replace with another medication, if necessary.