Table of Contents[Hide][Show]
- LISTEN TO THE PODCAST
- CHAPTERS
- Are the Diabetes Guidelines Keeping Up? Key Insights for Managing Type 2 Diabetes and Prediabetes
- 1. Carbohydrates: The Missing Clarity
- 2. Digital Programs: A Game-Changer in Diabetes Care
- 3. The Role of Sleep in Blood Sugar Management
- 4. B12 Deficiency and Metformin Use
- 5. The Power of a Balanced Eating Pattern
- 6. Fats and Proteins: Missteps in the Guidelines
- Moving Forward: Take Action Today
- Transcript
If you’re living with type 2 diabetes or prediabetes, you might have come across the American Diabetes Association (ADA) Standards of Care in Diabetes—a document updated annually to guide healthcare professionals in treating diabetes.
But are these guidelines truly helping people improve their health? In this episode, we’ll explore some of the key takeaways from the 2025 ADA guidelines, examining the evidence and advocating for clearer firmer guidelines on macronutrients, especially carbohydrates.
LISTEN TO THE PODCAST
CHAPTERS
1:16 ADA Standards of Medical Care overview
4:34 Digital programs outperform in-person care
6:37 Importance of sleep and monitoring B12 in prediabetes
8:46 Eating patterns and the totality of what you eat
11:52 FAIL: No clear carbohydrate recommendations
18:02 FAIL: No evidence that plant protein is better than animal protein
20:15 FAIL: Guidelines on fats regressed, not progressed
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
Are the Diabetes Guidelines Keeping Up? Key Insights for Managing Type 2 Diabetes and Prediabetes
The ADA guidelines aim to provide health professionals with evidence-based advice, but they don’t always hit the mark. This year’s guidelines, spanning a whopping 359 pages, acknowledge that reducing carbohydrate intake is critical for managing blood sugar.
Yet, they fail to offer clear definitions or benchmarks for carbohydrate intake, leaving healthcare providers and individuals alike confused about what “carbohydrate restriction,” “low carb,” “very low carb” or “ketogenic” actually means. Without actionable guidance, many of the recommendations are difficult to implement.
1. Carbohydrates: The Missing Clarity
In the 2025 guidelines, carbohydrates are recognized as the macronutrient with the greatest impact on blood sugar and A1c levels—that’s nothing new, we’ve know this for a very long time!
However, the ADA stops short of providing clear recommendations on carbohydrate ranges.
What does this mean for you?
Don’t listen to the ADA guidelines!
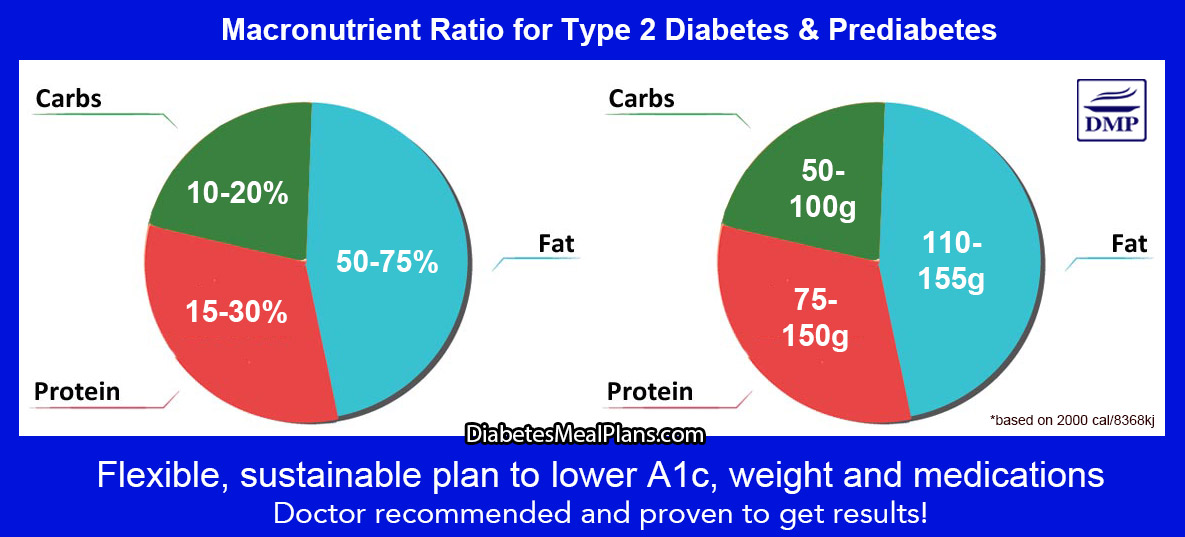
To make real progress in managing blood sugar, aim for 10-26% of your daily energy intake from carbohydrates, which translates to roughly 50-129 grams of carbohydrates per day on a 2,000-calorie diet.
This range is supported by ample research and provides enough flexibility to include nutrient-dense foods while reducing blood sugar spikes.
Even better, we’ve seen the following recommendations work best:
2. Digital Programs: A Game-Changer in Diabetes Care
One major improvement in recent years is the growing recognition of digital health programs.
Evidence now shows that digitally-delivered diabetes education and support—like telehealth or structured programs—are often more effective than in-person care.
Programs like our T2Diet Program have been clinically proven to reduce A1c, support weight loss, and lower medication use.
Why does this work?
Digital programs offer ongoing education and support, something you simply can’t get from a pamphlet or a one-time visit to your doctor.
Diabetes is a journey, and staying informed and supported is key to achieving lasting results.
The most important thing is finding a proven program, as many online programs are not proven to work, unlike our clinically proven T2Diet Program or VIP Membership.
3. The Role of Sleep in Blood Sugar Management
Did you know that poor sleep can significantly increase your risk of diabetes?
The 2025 guidelines highlight the importance of quality sleep in supporting metabolic and hormonal health. Sleep deprivation affects your entire system, from blood sugar levels to cardiovascular health.
What can you do?
Aim for 7-9 hours of sleep per night to give your body the rest it needs. If you’re struggling with sleep, try creating a consistent bedtime routine, limiting screen time before bed, and keeping your bedroom dark and cool.
4. B12 Deficiency and Metformin Use
If you’re taking metformin, one of the most common medications for prediabetes and type 2 diabetes, you should be aware of its link to vitamin B12 deficiency.
This deficiency can worsen symptoms of peripheral neuropathy, a common complication of diabetes.
Practical Advice:
Don’t wait for symptoms to appear—proactively monitor your B12 levels to stay ahead of any potential issues.
Ask your doctor to include a B12 test during your routine lab work. If your levels are low, B12 supplementation can help address the deficiency and potentially reduce the severity of neuropathy symptoms.
5. The Power of a Balanced Eating Pattern
The 2025 ADA guidelines emphasize the importance of overall eating patterns rather than focusing on individual nutrients.
While this shift is beneficial, they still fail to acknowledge the importance of educating people about macronutrients.
For those with type 2 diabetes or prediabetes, low carbohydrate eating patterns consistently show better results than other diets, such as the Mediterranean diet, for reversing blood sugar levels to normal.
What can you do?
Make small, sustainable changes to your eating pattern. Focus on a nutrient-dense eating plan that limits added sugars and processed foods.
Incorporate plenty of non-starchy vegetables, quality proteins, and healthy fats like nuts, seeds and olive oil.
Join the T2Diet Program or Prediabetes Reset Program so you don’t have to figure it all out for yourself!
6. Fats and Proteins: Missteps in the Guidelines
This year’s guidelines regress on dietary fats, advising people to limit saturated fats without providing strong evidence to support this recommendation.
Similarly, the shift from “strong evidence” in 2024 to “growing evidence” in 2025 about plant protein replacing animal protein highlights inconsistencies in the messaging.
What does this mean for you?
Our body needs all types of fats, so instead of fearing saturated fats, focus on whole, nutrient-dense foods.
Don’t shy away from healthy fats like full-fat dairy or butter, as these are healthy nutrient-dense foods.
Animal proteins are complete proteins, offering all nine essential amino acids, making them a valuable part of a balanced diet.
Since diabetes affects many people at older ages, protein is essential for maintaining muscle mass and cellular function.
Moving Forward: Take Action Today
The ADA guidelines offer a wealth of information, but as you’ve seen, they’re not without flaws.
By focusing on the practical steps outlined here, you can cut through the confusion and take meaningful strides in managing your health.
Remember, diabetes management isn’t about perfection—it’s about progress. Every small step you take brings you closer to better health.
If you’re ready to take charge of your health with evidence-based guidance and support, check out programs like the T2Diet Program or Prediabetes Reset Program, where we combine research with real-world results to help you succeed.
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful people, Dr Jedha here and welcome to episode 62 where we’ll be doing our annual investigation of the diabetes guidelines.
01:16
The American Diabetes Association, also known as ADA, releases the Standards of Care in Diabetes every year, which they have been doing since 1989. Other places around the world update their guidelines every 2-5 years, and usually they follow along with what the ADA guidelines recommend. Overall, we don’t tend to see a great deal of changes in the guidelines from year to year, although slowly we hope to see new evidence reflected in the guidelines.
The 2025 guidelines have a total of 359 pages, 31 more pages than 2024 and again, with thousands of references. Now, just because these guidelines include many thousands of references, doesn’t mean the included papers have been thoroughly reviewed for accuracy or quality. In fact, I’ve seen things quoted in the guidelines where clearly the ADA committee have only read the abstract and not the entire paper—that’s bad practice because it’s in the methods and results sections of papers that we find the true facts. What I’m trying to say is that the Standards of Medical Care can be flawed, depending on who is reviewing the evidence. With any evidence, we have to position it among everything else—all the other evidence available.
There are multiple chapters in the Standards of Medical Care so it’s difficult to get across all of them and I generally bounce around the chapters to assess any differences or if I’m looking at a particular thing. And of course, I always tend to focus on the chapter about facilitating behavior change, which focuses on nutrition.
We did a thorough investigation of the diabetes guidelines back in episode 9 where we included a more historical view of the guidelines as well, so you may be interested to listen to that episode for even more context on what we’ll discuss today.
The Standards of Care are designed for health professionals, to give them guidance so they can help their patients with diabetes improve their health, but as I noted in episode 9, the dietary guidelines are quite vague and unless you are prepared to go and do substantial research yourself, overall I’d think most health professionals wouldn’t find them very helpful. This year it’s equally the same, the guidelines are vague and in some ways I think, even more confusing. There’s still no clear benchmarks for macronutrient intake—which is your carbohydrates, protein and fat. There is clear confusion about dietary definitions, particularly surrounding carbohydrates. The dietary recommendations surrounding fat have seemed to regress and those on protein are largely unsubstantiated. Overall, with the evidence available on diet and nutrition, it raises the question about why ADA continues to hesitate to adopt firmer stances. We’re going to be diving into all this to investigate further.
04:34
Firstly I wanted to mention digital health programs. In 2020-21, there were still reservations regarding the effectiveness of digitally-delivered diabetes education. From 2023 onwards, there has been strong evidence for the benefits of digital support— and what we’re talking about here are things like telehealth or programs such as our clinically proven T2Diet Program or our VIP Memberships. The evidence shows these are more effective than in-person care for reducing A1c and leading to better health outcomes overall. There is no doubt about that. Let’s face it, it does not help to be given an outdated pamphlet at the doctor’s office—that’s not education. Diabetes education is an ongoing process. Any type of health journey requires ongoing education and support. Education is the cornerstone to making change. Ongoing support solidifies health goals. That’s why digital programs are so effective. Digital programs are convenient and you can access them any time to get the education and support you need. You can’t get that type of education and support with a pamphlet, or even with one visit to a healthcare professional. You need ongoing education and support, time to take it all in and implement it. So strong evidence now continues to exist for digitally-delivered programs and support—and I’m proud to say we are pioneers in terms of digital, as we have the only nutrition program worldwide clinically proven in a randomized controlled trial to reduce A1c, weight and medications.
06:37
For our listeners or members with prediabetes, we know that nutrition and diet are primary treatment strategies that can reverse prediabetes and prevent a type 2 diabetes diagnosis. Evidence continues to highlight this. Although nutrition is the central focus, it does go beyond what you eat, to making sure you do regular physical activity and the importance of sleep has now been added to the guidelines. Sleep is so incredibly important. Quality sleep is needed to support metabolic, hormonal and cardiovascular processes, so when we lack sleep it influences our entire metabolism and system. Studies have indicated a significant risk of diabetes with poor quality sleep. Research indicates you need to aim to get an average of 7 hours a day, not less than 6 hrs and not more than 9 hours.
If you’re taking Metformin, you should be aware that it can lead to vitamin B12 deficiency, an important point highlighted in the 2025 guidelines. If you do take metformin you need regular assessment of your B12 levels, which you can get via a simple blood test when you do your routine labs with your doctor. If you have peripheral neuropathy, you should be aware that B12 deficiency is related to this—people are often deficient and this can increase severity of pain and symptoms, so get tested for B12, and this is obviously more important if you’re taking Metformin and have peripheral neuropathy.
According to the guidelines, Mediterranean and low carbohydrate are the best diets to prevent type 2 diabetes. The evidence for lowering carbohydrates in your diet is stronger than Mediterranean for treating and reversing prediabetes to normal.
08:46
Moving on, let’s dig in to explore the dietary guidelines section in Chapter 5. Firstly let’s talk about eating patterns, then I’d like to shine a spotlight on one of the most debated and, frankly, confusing areas for people with diabetes and practitioners alike, and that is carbohydrate recommendations.
So firstly food patterns.
One of the important things we have learned in nutrition science over the years is that it’s your overall eating plan that makes the biggest difference to your long term health, not any one food you might eat. Of course we know based on evidence and logic that a healthy eating pattern, an eating plan that contains mostly nutrient dense whole foods and limits added sugar and processed foods is going to be a better eating plan for anyone.
The beginning of the 2025 guidelines for nutrition therapy states, and I quote:
“There has been a change in how we talk about nutrition. We are moving away from emphasizing macronutrients, which include carbohydrates, proteins and fats, and micronutrients, which include vitamins and minerals, and instead focusing on foods. More broadly we are encouraging people to think in terms of eating patterns also known as dietary patterns or food patterns, or the totality of foods and beverages a person consumes.”
This is true to a certain extent. As we just established, we know that if you have a healthy eating pattern, you’re going to be healthier. In contrast, if you have an unhealthy eating pattern you’re more likely to develop health concerns. That’s just logic and we don’t really need evidence to prove it but in any case there is an abundance of evidence that does prove it. But, for people with prediabetes and type 2 diabetes, it’s ignorant to think that educating people about macronutrients and micronutrients is not beneficial, and critically important. And when I read it this year, for some reason I couldn’t help thinking that it just all seems like an excuse for avoiding the provision of clearer guidelines and a firmer stance on macronutrients in particular.
11:52
When we get down to the nitty gritty, the guidelines have failed to provide anything solid, stating yet again that there is no ideal percentage of calories from carbohydrate, protein and fat for people with diabetes. This is absolutely not true, especially for carbohydrates. In fact, defining carbohydrates is where the confusion begins and perpetuates, with the guidelines continuing to provide no definitions. This is contradictory to the evidence, which is clear, and also acknowledged in the guidelines time and time again.
That’s right, the guidelines acknowledge that reducing carbohydrate intake improves glycemic control—a point that’s been consistent for years. Going right back to the 2005 guidelines we’ve always understood that carbohydrate is the macronutrient with the greatest impact on blood sugar and A1c levels—that fact continues to be acknowledged. The guidelines acknowledge that monitoring carbohydrate is the key strategy in reducing blood glucose. They acknowledge that the most effective eating patterns to reduce A1c and medications are low carbohydrate and very-low-carbohydrate eating patterns. And yet they fail to give any clear definitions about carbohydrate and that’s incredibly confusing.
The 2025 guidelines are made even more confusing for healthcare practitioners as they use various different terms for carbohydrate eating patterns – they used carbohydrate-restricted, low carbohydrate, very low carbohydrate, and ketogenic. They also mix up the terms using them interchangeably, when they are different and that is very confusing.
I’ve said it before and will say it again and again. The medical care guidelines need a clear definition of carbohydrate so that healthcare practitioners who read this actually have some proper guidelines to work within, and it’s not complicated. I published a paper in Diabetes Research and Clinical Practice back in 2020 with the consensus for clear definitions on carbohydrate intake, so let’s lay it out here and you can visit the show notes to view this.
Basing this on an average 2000 calorie a day intake. A ketogenic diet is less than 10% carbohydrate from total daily energy intake or below 50g carbs grams per day. Low carbohydrate diet is above 10% and below 26% carbohydrate from total daily energy intake, a range of 50-129 grams of carbs per day. A moderate carbohydrate diet is 26-45% carbohydrate from total daily energy intake or 130-225 grams of carbs per day. A high carb diet is above 45% carbohydrate from total daily energy intake or >225 grams of carbs per day.
The guidelines simply have to state something like this, but honestly, I don’t think they know what the definitions are themselves as they are all over the place. As an experienced researcher, it is absolutely essential to establish clear definitions, otherwise you cannot evaluate the evidence in a suitable fashion. There are many studies that say they are low carb within the title or discussion, when the carbohydrate intake is clearly in a moderate range—therefore, the study isn’t looking at a low carb diet and cannot be included in a discussion as such. This happens all the time and is one critical flaw when evaluating research.
Given nutrition is my area of expertise in practice and research, we know that there is a specific carbohydrate range that should be recommended, and it’s disappointing that it’s not included in the guidelines, again. The carbohydrate recommendation they should be including in the guidelines is that health professionals should recommend their patients consume under 26% carbohydrate from daily energy intake, full stop. That’s what all the research shows conclusively. Ketogenic diets can be effective, but the evidence shows that people have difficulty maintaining this level of carbohydrate restriction long term and there still remain concerns about lack of dietary fiber, excessive amounts of saturated fat and potential for vitamin and mineral deficiencies. Whereas low carbohydrate, 10-26% carbohydrate from daily energy intake, provides a wide variable to be able to construct a healthy low carb nutrition plan to meet all nutritional requirements. So basically, if the guidelines did specifically suggest that people consume 10-26% carbohydrate from daily energy intake, we’d see masses and masses of people changing their diabetes health, we certainly would.
When I read the wording, it’s almost as if the 2025 guidelines have regressed in terms of their carbohydrate emphasis from the previous 4 years of guidelines, which is a pity.
18:02
In terms of protein, there was an an addition in the 2024 guidelines that stated and I quote:
Strong evidence suggests higher plant protein intake and replacement of animal protein with plant protein is associated with lower risk of all-cause and cardiovascular mortality.
This was removed and replaced with this statement:
“Growing evidence suggests higher plant protein intake and replacement of animal protein with plant protein is associated with lower risk of all-cause and cardiovascular mortality.”
See how interesting that is. It’s gone from strong evidence in 2024, which if you listen to episode 9, was completely unfounded, as there was no strong evidence. And this year proves that as it states that there is growing evidence. Again, it’s weak evidence and overall there is no substantial evidence that suggests replacement of animal protein with plant protein is associated with lower risk of all-cause and cardiovascular mortality. The only justification provided and I quote is:
“Plant proteins are lower in saturated fat, higher in fiber, and also support planetary health.”
That’s not an adequate justification nutritionally. I’m not against eating plant protein, but nutritionally speaking, there is no evidence to suggest that replacing animal protein with plant protein is beneficial or leads to better health outcomes. We certainly need good quality protein to support so many critical functions in our bodies. Animal proteins are complete proteins as it’s only animal protein that provides all nine essential amino acids, plant-based proteins are incomplete as they lack all essential amino acids, so nutritionally speaking with protein, plant-based proteins are inferior.
20:15
In terms of fats, unfortunately the guidelines have regressed in this area as well, rather than progressing. In this years guidelines table 5.2 states, and I quote:
“Counsel people with diabetes and those at risk for diabetes to limit intake of foods high in saturated fat (e.g. red meat, full-fat dairy, butter and coconut oil) to help reduce cardiovascular disease risk.”
This is such outdated thinking and is not advice based on solid evidence. There is no explicit evidence provided regarding the limitation of saturated fat.There is no evidence provided for the foods mentioned either. In fact, in 2023, the guidelines suggested ‘dairy’ was fine. It wasn’t until 2024 that they suddenly switched to low-fat dairy, without any research to justify the change. Instead, this is just an outdated blanket statement based on the standard dietary guidelines, inaccurate guidelines that were never supported by evidence in the first place. Sad to see it regress to this yet again. And also, it just seemed like a strange attack on nutrient dense whole foods when the overarching focus was on food patterns and encouraging people to eat nutrient dense foods. Unfortunately deeply ingrained narratives are difficult to overcome, despite whether they are true or not. But being that guidelines should be based on evidence, this continues to disappoint.
Of course, with 359 pages to explore, we’ve only scratched the surface of the 2025 guidelines, but coming back to summarize this year’s investigation, not much has progressed in terms of dietary recommendations, and if anything, the guidelines appear to be regressing back to outdated thinking, rather than proper research and evidence.
As always, it’s vital to approach these guidelines with a critical lens, balancing what’s presented with the broader scope of evidence we have available. The lack of clarity and progress in areas like carbohydrate recommendations and dietary fats is disappointing, but it also reinforces the importance of seeking additional, high-quality sources of guidance for diabetes treatment, such as this podcast and the programs and services we provide at DMP.
At the end of the day, nutrition isn’t just about what’s written in guidelines—it’s about practical, evidence-based strategies that actually work, much of which gets buried in the sea of research and lost in unfounded dominating societal narratives that continue to perpetuate. Just because certain narratives dominate common thinking, doesn’t make them facts. That’s exactly why I’ll continue to deep dive into the research and continue to advocate for clear, actionable strategies that make a real difference in people’s lives.
Thank you for listening today and be sure to tune in next week.
Dr Jedha, over and out.
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…

Leave a Reply