Below is a summary of the American Diabetes Association (ADA) dietary treatment guidelines (Standards of Medical Care in Clinical Practice 2017) for adults with type 2 diabetes mellitus and how Diabetes Meal Plans (DMP) aims to meet, and assist providers and healthcare professionals to meet those clinical guidelines.

Uniting to support people’s health
It’s our duty as healthcare educators and professionals to guide people in a positive direction and provide them with the support and guidance they need to change habits.
One essential factor to recognize is that type 2 diabetes and prediabetes is largely a self-managed process. Therefore, people need to be enabled with knowledge, skills and tools to manage their condition.
One of the key areas they need to gain this knowledge and skill is around diet and food. Quite simply because healthful eating is one of the core elements of self-care behavior.
But, “for many individuals with diabetes, the most challenging part of the treatment plan is determining what to eat and following a food plan. (ADA S34).”
Quite frankly, most information on the web is too generic, difficult to understand, and overwhelming for the newly diagnosed, the long-term diabetic, and prediabetic people alike.
It is our duty to help guide them in a positive direction and provide education and resources that people can actually apply to their every day lives, which is exactly what we do here at DMP.
ADA recommends that “each person with diabetes be actively engaged in self-management, education, and treatment planning with his or her health care provider, which includes the collaborative development of an individualized eating plan.”
The overall objectives of education are to support:
- Informed decision making
- Self-care behaviors
- Problem solving
- Active collaboration with the health care team to improve clinical outcomes
- Improved health status and quality of life
“Unfortunately though, a large percentage of people with diabetes do not receive any structured diabetes education and/or nutrition therapy,” according to ADA.
And that is a large part of the problem we need to work together to solve.
Diabetes education usage stats
The stats on education usage in the United States:
- Only half of people diagnosed receive some type of education, fewer see a registered dietitian.
- Out of 18,404 diabetic patients only 9.1% had at least one visit for nutrition therapy in 9 years.
- Even though Medicare or insurance may cover people’s attendance to diabetes education sessions, only a small 5-7% of people utilize it – meaning, there is a big gap that needs to be filled.
Education can come in the form of contact with certified diabetes educators or healthcare providers, but it doesn’t have to. Independent organizations such as Diabetes Meal Plans, friends, family and peers all play an important role in supporting people to choose more positive actions.
The challenge for us as healthcare educators and providers is to overcome these barriers and help people with diabetes gain access to the knowledge, skills and tools they need to control their diabetes and live a healthy life.
The perfect time to guide them toward nutrition education is at diagnosis, but any point along their journey can spark the motivation to change. And it should also be noted that people with prediabetes are often overlooked. They too can be referred to nutrition education programs to help them improve their health and avoid a type 2 diabetes diagnosis.
The DMP team endeavors to do service to the public (people with type 2 diabetes and prediabetes) by taking complex information and making it easy-to-understand, and most importantly, making information practical so people can apply what they learn to their everyday life.
And combined, our evidence-based info and meal planning tools and support service help people overcome these challenges, especially being that everything we provide is Internet-based, making it convenient and accessible to people worldwide.
Emerging evidence demonstrates the benefits of Internet-based programs and the need for innovation in healthcare. And the ADA suggests innovative models need to be explored, which is why we’ve created Internet-based programs and tools.
Our goal is to partner with healthcare educators and providers to improve people’s lives because we know that together we can help make a difference.
The right type of diet
Diabetes organizations worldwide agree that there is no one-size-fits-all dietary plan and that many dietary patterns can work. Any whole foods based eating plan has the potential to offer improved health to people with diabetes and prediabetes.
However, every organization also agrees that the AMOUNT of carbohydrates an individual eats has the greatest impact on blood glucose control. This is simple biochemistry that every health professional or researcher understands.
With this in mind it’s no surprise that emerging evidence continues to demonstrate that low carbohydrate diets are an effective tool for managing diabetes. Therefore, DMP encourages a low carbohydrate Mediterranean-style food plan that aligns with current research and American Diabetes Association (ADA) guidelines.
ADA’s 4 Goals of Nutrition Therapy for Adults With Diabetes
1. To promote and support healthful eating patterns, emphasizing a variety of nutrient-dense foods in appropriate portion sizes, in order to improve overall health and specifically to:
- Achieve and maintain body weight goals
- Attain individualized glycemic, blood pressure, and lipid goals
- Delay or prevent the complications of diabetes
2. To address individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthful foods, willingness and ability to make behavioral changes, and barriers to change
3. To maintain the pleasure of eating by providing nonjudgmental messages about food choices
4. To provide an individual with diabetes the practical tools for developing healthy eating patterns rather than focusing on individual macronutrients, micronutrients, or single foods
Additionally, there should also be a long term view to encourage people to sustain an improved lifestyle.
And just to be clear, both nutrition and lifestyle change are equally important whether a person is taking medications or not.
Our dietary philosophy
Our nutrition education focuses on a low carbohydrate Mediterranean-style food plan that aligns with current research and ADA’s guidelines.
ADA’s position statement concludes (published in Diabetes Care): “Nutrition interventions should emphasize a variety of minimally processed nutrient-dense foods in appropriate portion sizes as part of a healthful eating pattern and provide the individual with diabetes with practical tools for day-to-day food plan and behavior change that can be maintained over the long term.”
We educate people about whole food intake:
- A high intake of non-starchy vegetables
- The inclusion of lean protein sources
- Choosing monounsaturated fat as the predominant dietary fat
- A moderate intake of lower carb fruits
- Along with nuts, seeds, dairy products and other whole foods
But we don’t just educate. We provide the knowledge, skills and tools in an easy-to-understand way. And most importantly, we make it practical so that people can apply what they learn to their lives.
And we are proud to say our members and subscribers are getting great results.
- Higher level of skill and ability in making food choices
- Improved dietary behaviors
- Psychological and emotional empowerment
- Lower blood glucose and A1c
- Weight loss
Carbohydrates
“Studies examining the ideal amount of carbohydrate intake for people with diabetes are inconclusive,” according to ADA.
However, it is well understood that while the type of carbohydrate is important, for instance, encouraging the selection of non-starchy vegetables over starch-based carbs. The AMOUNT of carbohydrates is the most critical factor that determines glucose and insulin response.
In which case, the universal recommendation is that monitoring carbs/ carb counting remains a key strategy for people to achieve good control.
The challenge here is that people don’t understand the group of carbohydrate foods because most information is very generic or confusing. And if/when they do understand the foods, they still struggle to put those foods together in a recipe or meal plan.
Our T2Diet Program takes people step-by-step through the group of carbohydrate foods and provides various options and alternatives to switch to better options. The program is designed to help people overcome these challenges.
The added challenge is that many carbohydrate foods promoted as ‘healthy’ to the general public are not well suited for diabetes treatment. This is one area many professionals come unstuck with their recommendations to people with type 2 diabetes or prediabetes.
For example, whole grains. While there is evidence to show whole grain intake may help reduce risk of diabetes. According to ADA, “whole-grain consumption is not associated with improvements in glycemic control in type 2 diabetes.”
Of course this makes sense because whole grains are carb-heavy. For instance, one cup of brown rice contains 46 grams carbs, while one cup broccoli contains just 6 grams. And despite commonly held assumptions, adequate dietary fiber can be obtained from consuming lower carb vegetables, along with nuts and seeds.
For instance, that some cup of broccoli contains 2.4 grams of fiber, while brown rice provides 3.5 grams.
Emerging evidence continues to demonstrate that a low carbohydrate approach is an effective way to control diabetes, consistently producing the following results:
- A1c reduction
- Immediate drop in fasting glucose levels
- Lower medication use
- Lower risk of hypoglycemia
- Decreased triglycerides and increased HDL
The ADA, Diabetes Australia and Diabetes UK now acknowledge that a low carb dietary pattern can help with diabetes management, a big change since 2015 when they were all largely against the dietary pattern.
So what is considered low carb?
A typical Western low fat diet recommends 50-60% carbohydrates. A low carbohydrate diet is considered anything below 130 grams per day, or below 26% of total calories.
A low carb diet is not to be confused with a ketogenic diet, which is below 10% of caloric intake. DMP is not a ketogenic website.
And surprisingly, even modest decreases in carbs (20-40% of total calories) can provide benefits for people with type 2 diabetes and prediabetes.
The point is, people need to know what the right types of carbs are and how to use them in recipes and meal plans. And that’s what we endeavor to do here at DMP.
If you are a physician or healthcare professional and people you work with choose to follow a low carb diet, it is important to support their dietary choice and assist them with reducing/ adjusting medications where needed.
It should also be noted that the ADA recommends, “for individuals on a fixed daily insulin schedule, meal planning should emphasize a relatively fixed carbohydrate consumption pattern with respect to both time and amount. By contrast, a simpler diabetes meal planning approach emphasizing portion control and healthful food choices” is best for most people.
To make those healthful carbohydrate food choices, people need education across the wide range of carbohydrate foods – complex and simple carbs, non-starchy vegetables as carbs, starches, sugar, fructose, fruit and so forth.
Our T2Diet Program addresses all these aspects and takes it one step further by providing options and alternatives so people know what to swap their high carb foods for. This provides them with real life tools to enable the practical every day application of a low carb eating plan.
Fat
According to the ADA, “Data on the ideal total dietary fat content for people with diabetes are inconclusive. An eating plan emphasizing elements of a Mediterranean-style diet rich in monounsaturated fats may improve glucose metabolism and lower CVD risk and can be an effective alternative to a diet low in total fat but relatively high in carbohydrates.”
We have a Definitive Guide to Fat for Diabetes over here.
The basic overview on fat is that:
- Artificially produced trans fats found in fast foods, bakery products and margarine etc, are bad for health outcomes
- Saturated fat should be kept to 10% of overall daily calories
- Follow the general dietary guidelines to consume lean sources of meat
- Keep processed meats to a minimum
- Dairy products, including full fat varieties are safe to consume
- Consume more omega 3-rich polyunsaturated fats
- Minimize omega-6 proinflammatory polyunsaturated fats
- Consume ample monounsaturated fats
It should be recognized that people who consume a low carb diet will naturally have a higher intake of fat, as an overall percentage of calories.
For instance, if people remove high carb foods like bread, pasta, rice and potatoes, people suddenly have a calorie deficit. They can increase the amount of vegetables they eat but they are relatively low in overall calories.
So the natural consequence is they eat more healthy fat sources. Not bacon and pork rinds as might be recommended on many low carb recipe sites, we certainly do not suggest people do that. But healthy fats like nuts, seeds, olives, avocado and olive oil – fats with proven health benefits.
As a natural consequence of reducing calories from high carb foods, healthy fat sources are generally increased.
The ADA supports this view and recommends that “when looking at metabolic goals and cardiovascular disease risk, the type of fats consumed is more important than the total amount of fat.” Monounsaturated and omega 3 fats are considered the best type of fats to include, and that’s what we adhere to here at DMP.
Protein
According to the ADA, “Research is inconclusive regarding the ideal amount of dietary protein to optimize either glycemic control or CVD risk. Some research has found successful management of type 2 diabetes with meal plans including slightly higher levels of protein (20–30%), which may contribute to increased satiety.”
A small randomized crossover trial (2004) in people with type 2 diabetes consuming 30% protein found that it had positive effects on A1c and insulin, reducing their levels significantly.
A study (2014) conducted over a 12 month period with type 2 diabetics who had kidney dysfunction compared a 30% protein intake to a standard 20% protein intake to see if it made any difference to weight loss, renal function (kidneys), or metabolic parameters. The study showed that the higher protein diet had no adverse effects at all, having comparable outcomes to the standard 20% protein diet.
A more recent study (2017) compared 30% protein from either animal or plant sources in type 2 diabetic patients over 6 weeks. The results showed that consuming 30% animal protein decreased inflammation and uric acid, improved insulin sensitivity and blood glucose control.
Meta analysis of low protein diets have shown no beneficial renal effects in diabetic patients.
The ADA suggests no lower intake is needed for people with kidney issues, while the Canadian Association suggests that in people with kidney issues it may be worth considering restricting protein intake at 0.8 g/kg body weight/day.
Overall the consensus is that the most important factor is choosing quality protein sources.
Sodium
According to the ADA, “As for the general population, people with diabetes should limit their sodium consumption to 2,300 mg/day.”
By encouraging people to consume fresh, natural whole foods, the addition of “added” salt in the diet is naturally resolved and frequently eliminates these issues.
Alcohol
As for the general population, people with diabetes should limit their intake of alcohol to one standard glass for women, two for men.
Sugar Substitutes
It is obviously recommended that sugar and sugar-sweetened beverages are eliminated. But since many people enjoy sweets, nonnutritive sweeteners can make a good substitute.
However, research shows that artificial sweeteners may increase risk of obesity, diabetes and insulin resistance. Whereas, safer options for people with diabetes/prediabetes are stevia, monk fruit, xylitol, erythritol and tagatose.
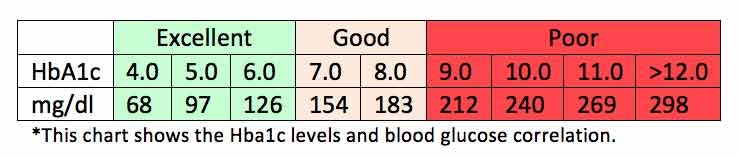
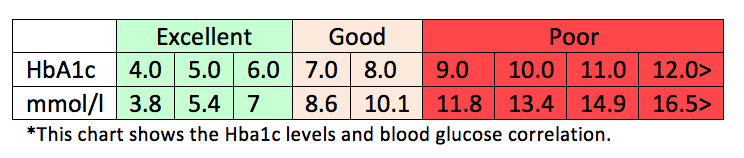
Glycemic targets
Self-monitoring of blood glucose levels provides people with accountability and is a useful tool for both you, as their healthcare provider, and them to evaluate how effective their diet, exercise, medication regime is working.
Obviously in those on insulin therapy, self-monitoring is more essential. However, even in those with type 2 diabetes who are taking oral medications such as metformin, or whom are not taking any medications, and even people with prediabetes, can benefit from self-monitoring.
Self-monitoring goals should be discussed between the patient and the healthcare team. But generally, fasting and before/after meals can be helpful. The overall goal is to reduce hyperglycemia and achieve healthy target ranges for blood glucose and A1c.
Depending where you live in the world, numbers can vary slightly. However, the generally agreed upon diagnostic ranges are as follows:
Normal Blood Sugar Levels
Fasting glucose – 70-99 mg/dl or 4-6 mmol/l (Note: there is some debate about the normal range in mmol/l, ranging from 5.5 to 6 mmol/l)
2 hours post meal glucose – less than 140 mg/dl or less than 7.8 mmol/l
Pre-diabetes – also called impaired fasting glucose or impaired glucose tolerance
Fasting glucose – 100-125 mg/dl or 6.1-6.9 mmol/l
2 hours post meal glucose level – 140-199 mg/ dl or 7.8-11 mmol/l
Diabetes
Fasting glucose – More than 126 mg/dl or more than 7.0 mmol/l
2 hours glucose level – More than 200 mg/dl or more than 11.1 mmol/l
Diabetes Blood Sugar Level Goals
Upon waking before breakfast (Fasting)
- 70-130 (Ideal under 110) mg/dl
- 4-7.2 (Ideal under under 6.1) mmol/l
Two hours after meals
- Under 180 (Ideal is under 140) mg/dl
- Under 10 (Ideal is under 7.8) mmol/l
Bedtime
- 90-150 mg/dl
- 5-8.3 mmol/l
The above levels, for people diagnosed with type 2 diabetes, are the general goals set by the American Diabetes Association and the American Association of Clinical Endocrinologists.
As suggested earlier, there is some variation in the blood sugar levels goals set by different organizations. So it’s up to healthcare teams to work with individuals to set appropriate goals that gradually move toward a more optimal healthy range.
For instance, fasting levels:
- Between 70-100 mg/dL or 4-5.6 mmol/l (optimal)
- 70-110 mg/dL or 4-6 mmol/l (still good control)
- 70-130 mg/dL or 4-7.2 mmol/l (more liberal, but realistic for many)
Prediabetes and Type 2 Diabetes Blood Sugar Level Goals Long Term
Ultimately it is recommended to encourage people to attain and maintain blood sugar levels within the healthy “normal” range.
- Fasting glucose – 70-99 mg/dl or 4-6 mmol/l. Note: there is some debate about the normal range in mmol/l, ranging from 5.5 to 6 mmol/l, the lower goal of 5.5 mmol/l is where the ADA sets it.
- 2 hours post meal glucose – <140 mg/dL or <7.8 mmol/l
People should also be encouraged to record their numbers so they can take actions to improve them. They should also be advised that monitoring glucose alone will not improve blood sugar or A1c outcomes. The numbers have to be used in conjunction with diet and lifestyle changes in order to get results.
We educate people about this in T2Diet Program.
The ADA also advises that physicians should “perform the A1C test at least two times a year in patients who are meeting treatment goals (and who have stable glycemic control). And perform the A1C test quarterly in patients whose therapy has changed or who are not meeting glycemic goals.”
Lifestyle modification
For people with prediabetes, behavior and lifestyle intervention is recommended with the goal of achieving 7% weight loss, at a pace of 1-2 pounds (0.5-1 kg) per week. “Lifestyle intervention could reduce the incidence of type 2 diabetes by 58% over 3 years. (ADA S44)”
Of course, a major factor in lifestyle modification is improvement in diet and nutrition.
Exercise of around 150 minutes a week is recommended for people with type 2 diabetes and prediabetes.
The ADA recommends, “Technology-assisted tools including Internet-based social networks, distance learning, DVD-based content, and mobile applications may be useful elements of effective lifestyle modification to prevent diabetes.”
Our 30 Day Turnaround Program and our weekly meal plans are Internet-based education programs.
Our patient education program
We know the biggest challenge people with type 2 diabetes and prediabetes face is determining what to eat and following a food plan.
The T2Diet Program helps people overcome these challenges by providing nutrition education in an easy-to-understand way that empowers the individual to make informed choices.
Our goal is to partner with you and your patients to optimize nutrition and lifestyle goals and health outcomes – to help your patients gain control of their type 2 diabetes or prediabetes.
TESTIMONIAL: “I learned I don’t have to live in fear of diabetes, but can take my power back and be proactive about it. I feel very upbeat and positive about eating habits being modified and changed without feeling deprived or like a victim.” — Sandra T.
Interested in referring patients to us?
Click here to learn more and register your interest.
We look forward to working with you because together we can help make a difference in people’s lives!
You can find further practice guidelines in the American Diabetes Association report.


NICOLAOS MYLONAS
Dear friends!
I am Nikolaos Milonas I am 70 years old and I live in Greece. I congratulate you for your Website. And I am one of the victims of Diabetes.
My regular occupation is an Agricultural Specialist in Plant Nutrition and I retired in this capacity.
As an agronomist I noticed that all Plant Problems come from poor nutrition. when the plants had the necessary data, they could face the various attacks from endogenous and exogenous agents with various mechanisms.
What I was excited about is that for any problem plants warn us before the problem becomes permanent and begins to cause permanent alterations and disasters.
As a Retiree, I began to study the human body and the Nutrition.
I noticed that it does not differ greatly from plant nutrition.
And the human body uses the same elements as plants. Uses all the items listed in the Mendelegief Directory.
As the Father of Medicine Hippocrates used to say thousands of years ago, “…. All coexist! and the good and the bad and the bitter and the sweet and the salty … “. they should all coexist with harmony but at the same time compete with each other.
If someone, for some reason, prevails then there will be a problem. If the problem is not corrected then damage will occur.
If the Damages are not corrected, then the problem will become chronic or permanent, followed by inflammation, illness, and worse cancer or other dangerous disease.
What you need to know is that the Agency has the mechanisms to return to normal rates, provided of course we give it the necessary to activate rehabilitation mechanisms.
We live in the Planet of Chemistry! The human body is the finest Biochemical Factory, which operates nonstop day and night. If he stops doing his chemicals then we will die.
If we do not give him the necessary information, then he will definitely use the waste from his operation or steal elements from other parts of the body with serious consequences for Health.
For 4 years I have been studying Eastern Medicine and Pain Management, combining them with Ancient Greek Medicine and Botanical Use and the Mediterranean Diet.
Jedha
It’s very true Nicolaos, the human body is a natural biochemical entity. And if we feed it natural food that nourishes the cells, problems can be corrected, just like plants!
jim
I am not a health care professional; just a patient who feels thoroughly disgusted with the professionals I see. I was officially diagnosed 2 years ago and probably could have been diagnosed 2 years before that. I can’t remember how long ago pre-diabetic was mentioned. I do wish way back when that somebody had handed me a pamphlet or something that explained the consequences of not doing something. Maybe they tried and I was too dense to recognize it, but I don’t think so. As I was reading this I could hear a commercial in the other room for a diabetes medication. The gist of it is an interviewer is asking how their type 2 affects their heart. “It doesn’t does it?” Every time I hear it I yell at the television that none of my professionals has yet told me.
OK, rant over! Thank you, thank you, thank you Elizabeth and Jedha for the information you give us. I believe you are not only educating properly, you are extending lives!
Jedha
Well said Jim and this is something I’ve heard a lot over the years. People are ignorant, even many health professionals. They just don’t understand the disease. And perhaps in many cases, they don’t understand the seriousness of it either.
I think Elizabeth and I have probably done more research on diabetes than many of them combined. But it’s difficult when you’re in private practice etc. That’s why our next endeavor is to take our 30 Day Turnaround Program to doctors and professionals. We want to educate as many people as possible so that they can ‘extend their lives’ – that’s exactly what diet and lifestyle changes can do!
We’ll soon have some handouts and we’ll be looking to people like you to hand them to your doctors. Hopefully together we can help make a difference to many peoples lives!