No doubt at some point during your prediabetes or type 2 diabetes diagnosis or treatment, you’ve been required to have a fasting blood sugar test in the clinic or conducted one at home yourself.
It goes without saying that, a major part of successfully managing your prediabetes or type 2 diabetes is knowing your numbers!
Your numbers are a key indicator of how well you’re doing overall. And they can help you and your healthcare team make key decisions about what needs to be changed or improved.
Still we know it can be confusing to know which numbers and tests are what. And more importantly, what those numbers mean to you.
So let’s explore the various fasting blood sugar tests now.
Blood sugar vs blood glucose
If you’re new to this, you may be wondering what the difference is between ‘blood sugar’ and ‘blood glucose’ and the answer is nothing.
Both terms are used interchangeably to refer to the same things.
So now that we’ve cleared up any confusion…
In-Clinic Tests
Some blood tests occur in the clinic that the doctor orders. The doctor may use these tests for either diagnosis or check-ups.
The basic procedure is: blood will be drawn from a vein using a needle and results will not be available to you until several days after your test.
So now, onto the variety of tests that may be conducted.
Hemoglobin A1c (A1c)
Technically, you’re not required to fast for an A1c test, but because it’s often taken alongside other tests, you’ll likely be fasting when you have it.
Hemoglobin is a protein component of your red blood cells.
Sugar (glucose) will attach itself to the hemoglobin protein, and this process is called glycation.
The A1c test measures how much glycation has occurred on your red blood cells, and therefore, provides a picture of how much sugar has been floating around in your blood. Because red blood cells die every 3 months, the A1c test reflects the average blood sugar value over the last 3 months.
When you receive your result for the hemoglobin A1c test (often shortened to A1c or HbA1c), it will be written as a percent (%). Use this chart below to better understand what the percent means.
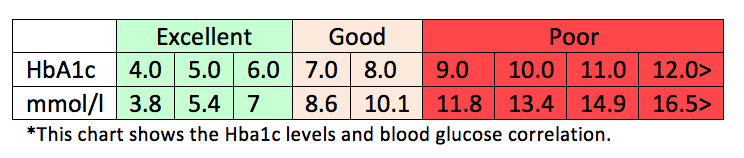
The normal range is between 4-6%.
Though note: Depending where you live in the world, A1c may differ slightly. For instance, “normal” A1c in US is considered under 5.7%. In the UK and Australia it is under 6%. Therefore, the generally recognized “normal” A1c range is between 4-6%.
If your A1c results came back above 5.7% (US), or 6% (UK, Canada & Aus) you may be diagnosed with prediabetes.
Whereas, if your results came back above 6.5%, you may be diagnosed with type 2 diabetes.
Your overall goal is to lower your A1c so it’s as close to normal as possible (4-6%). Though sometimes your healthcare team may set your goals slightly higher, for instance, 7%.
Remember, A1c is an average value of your blood sugar readings over the past 3 months. Doctors will typically order this test anywhere from 1 to 4 times throughout the year.
Fasting Blood Glucose
While technically you do not need to fast for the above mentioned A1c test, almost always your doctor will order a fasting blood glucose test to accompany it.
In order to get true results, you will need to consume your last meal at least 8 hours prior to when you plan to have the blood drawn (it can be longer).
Water is the only thing allowed to be consumed leading up to your test. In fact, it’s recommended you come to your appointment well-hydrated because it makes the veins easier to find.
The goal for fasting blood sugar may vary depending on the recommending organization, but generally this is a good guide to follow:
- Between 70-100 mg/dL or 4-5.6 mmol/l (optimal)
- 70-110 mg/dL or 4-6 mmol/l (still good control)
- 70-130 mg/dL or 4-7.2 mmol/l (more liberal, but realistic for many)
Glucose Tolerance Test (GTT)
A glucose tolerance test will look at how your body responds to consuming sugar, and may take up to 3 hours to complete.
First, you will need to fast for this test too, so you may choose to schedule this test in the morning after completing an overnight fast.
When you arrive to the clinic, you will drink a syrupy drink that contains about 75 grams of carbohydrate. Then your blood sugar levels will be checked every 30 to 60 minutes, for up to 2 hours.
The final number collected at hour two will let your physician and you know how well your body can process (tolerate) glucose.
Interpret the numbers as follows:
- Normal: Less than 140 mg/dL / Less than 7.8 mmol/l
- Impaired Glucose Tolerance: Between 140 mg/dL – 199 mg/dL / Between 7.8 mmo/l – 11 mmol/l
- Diabetes: Greater than 200 mg/dL / Greater than 11.1 mmol/l
Impaired Glucose Tolerance (often termed IGT) means that your body is not tolerating glucose as well as it could. This is also termed as prediabetes.
If you know the results of your GTT put you into the impaired glucose tolerance/ prediabetes group, then it is important to make appropriate diet and lifestyle changes as soon as possible, to prevent the onset of type 2 diabetes.
Please pin, tweet or share; then keep on reading.
At-Home Tests
Realize that there are also some tests that occur at home.
Any time you use a blood glucose monitor, you are conducting a blood test to better understand and manage your blood sugar levels.
Unlike the tests in the doctor’s office, these in-home tests use a finger prick to collect a sample and the results are available instantly.
Fasting Blood Glucose
A good practice for many people is to check blood sugar levels first thing in the morning using your glucose monitor. This is also called your fasting blood sugar levels.
The same fasting procedures for the in-clinic fasting blood glucose test above, hold true for this in-home version of the fasting blood sugar test as well. For the value to be considered fasting, you must have consumed your last meal at least 8 hours prior to the collected value.
Keep your supplies by your night stand, bathroom, or kitchen counter so that a quick check in the morning can easily become part of your morning routine.
In terms of goals for fasting levels, the same applies whether you’re at-home or in-clinic:
- Between 70-100 mg/dL or 4-5.6 mmol/l (optimal)
- 70-110 mg/dL or 4-6 mmol/l (still good control)
- 70-130 mg/dL or 4-7.2 mmol/l (more liberal, but realistic for many)
Why are fasting levels high in diabetes?
This is a common question and to help answer this question, please refer to the following resources:
- The dawn phenomenon – reason behind morning levels
- Fasting levels FAQs
- Tips to lower morning levels
Conclusion
To recap, there are some tests that will occur in a lab or doctor’s office where blood will be drawn by a professional.
But, you also have your own responsibility to check your blood sugar levels at home and interpret what these values mean. In fact, keeping a regular log of your levels can help you identify how you’re going in terms of blood sugar management, so you and your healthcare team can make decisions about what needs improving.
One important concept to understand is the difference between blood sugar levels and A1c.
Remember:
- Blood sugar = daily readings that show more fluctuation because blood glucose levels are affected by diet, sleep, stress, exercise and so forth.
- Hemoglobin A1C = an average reading of three months that is not influenced by the above daily factors.
Both tests are often used together to help provide a clearer picture of what’s occurring in your body.
Having good control of your blood sugar is crucial for long term health and preventing any potential complications from occurring.
Start with a healthy diet and lifestyle, and medication as needed, to bring your numbers into a healthy range.

Joe
This is great information! Thank you!
Debbie
Emily
When do you start the clock for the two hours blood draw after a meal? Is it when you put the first piece of food in your mouth at the beginning or when you are done eating your whole meal? And can you tell me the why behind the reason of your choice.
Thank you
Debbie
Emily - Dietitian (MS, RD)
Hi Debbie, First bite of food! This is when digestion starts, prompting the insulin response, which ideally runs it course within those two hours. There is some more information about the postprandial meal test over here.