For years, obesity has been diagnosed using a simple measure called Body Mass Index (BMI). If you’ve been told your BMI puts you in a certain category, you might have felt confused, judged or even misunderstood.
But what if there’s a better way to define health—one that focuses on how your body functions, rather than just your weight and height?
A new report from The Lancet Diabetes & Endocrinology, published on 15 January 2025, is challenging traditional thinking about obesity and offering new ways to improve care for people.
Overall, this is a positive move, as we’ve known for a very long time that BMI alone is not a good indicator of obesity or overall health.
Why BMI Doesn’t Tell the Full Story
BMI has been the standard for diagnosing obesity because it’s simple and quick. Take a look at this ‘standard traditional’ BMI categorization.
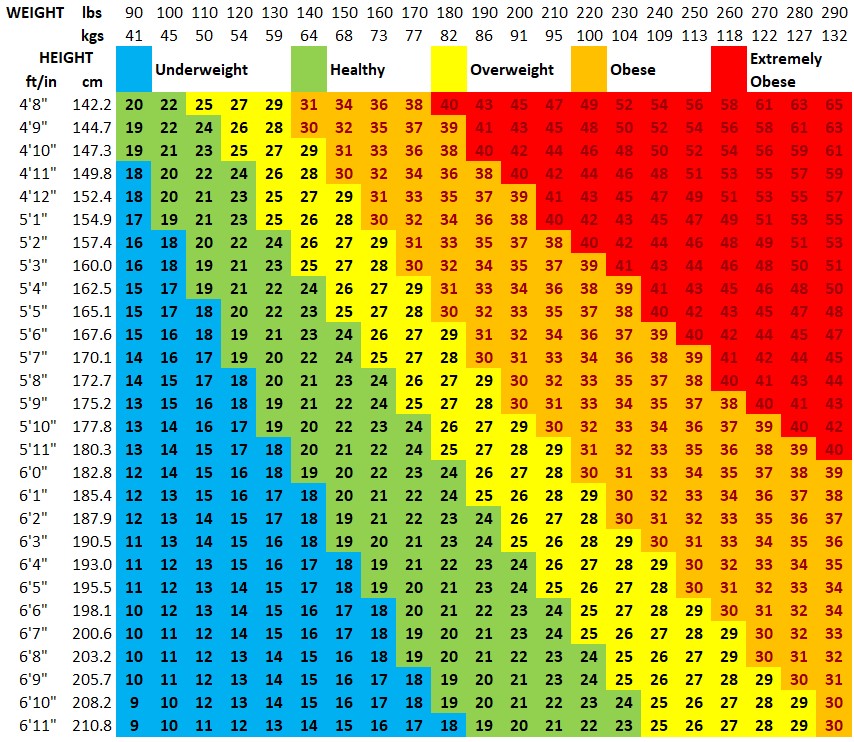
There’s one major downfall with this: BMI doesn’t distinguish between fat and muscle, nor does it consider where fat is stored.
This matters because fat around your organs—such as your liver or heart—is far more dangerous than fat stored in other areas like your arms or legs.
For example, someone with a “normal” BMI could still have significant health risks if they have visceral fat (fat around the belly and organs), while someone classified as “obese” might not have any related health problems.
Relying on BMI alone means that many people may be diagnosed as ‘obese’ when they are not—an over-diagnosis of obesity.
Plus, relying on BMI alone often overlooks critical health details, such as how fat distribution affects insulin resistance and overall health.
A New Way to Understand Obesity
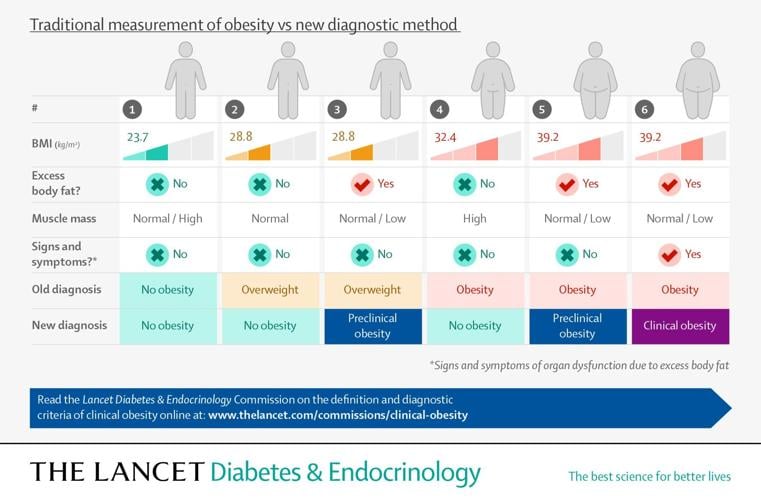
The Lancet Commission has introduced two new categories to better define obesity:
- Preclinical Obesity: This refers to excess body fat without current damage to organs or limitations in daily activities. However, it comes with an increased risk of developing type 2 diabetes, cardiovascular disease or certain cancers.
- Clinical Obesity: This is when excess body fat has already started to damage organs or limit your ability to carry out daily activities, like walking or getting dressed. This makes it a chronic illness, not just a risk factor.
New Tools to Assess Your Health
Instead of just looking at BMI, this new approach uses other tools to assess your health risks.
Here’s what they involve and how you can measure them:
- Waist Circumference (WC)
- What it measures: The amount of fat stored around your abdomen, which is strongly linked to health risks like insulin resistance and cardiovascular disease.
- How to measure: Use a tape measure to wrap around your waist, just above your hip bones and below your ribcage (usually at the level of your belly button). Make sure the tape is snug but not compressing your skin.
- Healthy numbers:
- Men: Less than 102 cm (40 inches)
- Women: Less than 88 cm (35 inches)
- Waist-to-Hip Ratio (WHR)
- What it measures: The proportion of fat stored around your waist compared to your hips. A higher ratio indicates more fat around your abdomen, increasing health risks.
- How to measure: Measure your waist circumference (as described above). Then, measure your hips at their widest point. Divide your waist measurement by your hip measurement.
- Healthy numbers:
- Men: Less than 0.90
- Women: Less than 0.85
- Waist-to-Height Ratio (WHtR)
- What it measures: The proportion of your waist size compared to your height, which can predict health risks more accurately than BMI in some cases.
- How to measure: Measure your waist circumference and divide it by your height (in the same units, either cm or inches).
- Healthy numbers:
- A ratio below 0.50 is generally considered low risk for both men and women.
These tools offer a much clearer picture of fat distribution and its impact on your health.
For example, your waist may be higher than the numbers indicated above but if your Waist-to-Hip Ratio and Waist-to-Height Ratio are fine, you will not be classified with obesity.
Limitations to the New Criteria
While these new criteria do provide a positive way forward, they still present inaccuracies and potential for misdiagnosis.
According to the new guidelines, your doctor or health professional should use one of the following to determine obesity.
- At least one of the body size measurements above, WC, WHR or WHtR
- At least two of body size measurements above, regardless of BMI
- Direct body fat measurements, such as DEXA scan
These criteria can still fail.
We ran and experiment with two healthy active people both of whom exercise daily, eat very healthy diets, have no diabetes or other health conditions and take no medication.
First, we used test number 1: only one measurement (waist circumference) and the ‘standard traditional’ BMI.
Interestingly, both of these people (women) had greater waist circumference than 88 cm (35 inches), so using that and BMI only, these women would still be classified ‘Preclinical Obesity’ according to the new criteria—given their good health, that’s just crazy!
But, if we used test number 2: Waist-to-Hip Ratio and Waist-to-Height Ratio, both women have very healthy fat distribution and would NOT be classified ‘Preclinical Obesity.’
Certainly, these new criteria can be more effective than BMI alone, but there are still limitations and flaws that could lead to misdiagnosis, which is why it’s also important to consider a person’s overall health as well.
Potential Downfalls of this New Obesity Criteria
Another potential downfall that concerns us is over-medicalization of obesity, which has happened with prediabetes and other conditions.
As a consequence of over-medicalization, what tends to happen is more people get put on medication when medication is not necessary.
What’s noted in the treatment of ‘Preclinical Obesity’ are ‘active weight loss interventions.’
Early interventions for preclinical obesity can help you avoid more serious issues, while targeted treatments for clinical obesity can restore organ function and improve your quality of life.
Hopefully though, on all fronts, this means health practitioners will recommend nutrition and diet as the primary treatment strategy, along with exercise before ever considering medication, as this is the most effective way to lose weight and keep it off long term.
What This Means for You
This redefined approach can make a big difference in how obesity—and your health—is managed:
- Personalized Care: If you’re in the preclinical stage, you can focus on lifestyle changes like a quality nutrition plan, physical activity, and blood sugar monitoring to prevent progression to a more serious health condition. If you’re already experiencing complications, targeted treatments that address multiple factors may be needed, but your focus should still be on a good diet plan.
- Reduced Stigma: Obesity is now recognized as a complex condition influenced by factors like genetics, hormones and lifestyle—not just a lack of willpower. This shift helps reduce judgment and encourages better support from healthcare providers, which we desperately need, as healthcare stigma and judgement is rampant.
- Improved Outcomes: By focusing on your individual health risks and needs, this approach prioritizes solutions that are tailored to you, whether that’s preventing complications or reversing existing damage.
But, you’re only going to get better outcomes if you were diagnosed accurately in the first place, so it is important to be aware of the limitations of the new diagnostic criteria, as we pointed out above.
It is also important to advocate for yourself. If doctors prescribe medication and you don’t want to take it, you need to say so. In many cases, medication is not needed.
A Focus on What Matters
Living with type 2 diabetes or prediabetes often means navigating conflicting advice about weight and health.
Your health is about more than a BMI score or number on the scale. It’s about how your body functions and how you feel each day.
Overall, we’re hoping this new way of defining obesity helps shift the focus to what truly matters: genuine care that focuses on improving your overall health long term.
If you need help to lose weight or achieve the best health, consider joining us as a member.


Leave a Reply