Hemoglobin A1c levels, sometimes referred to as A1c or HbA1c, is an often confusing topic for many. And that’s exactly why we’re going to cover a bunch of questions in the discussion below.
If you have questions of your own, please leave them at the bottom and join the discussion.

What does A1c mean and how is it calculated?
Hemoglobin A1c is “glycated hemoglobin.”
Hemoglobin is a protein found in red blood cells whose job is to carry oxygen to the cells. As it does so, it comes in contact with other components in the bloodstream, including sugar (glucose). When sugar gets attached to a protein, it’s called “glycation.”
The greater the glycation, the more reflective that is of sugar content in the bloodstream. Because red blood cells turn over every 3 months, measuring HbA1c gives us a 3 month average of blood sugar control. The A1c is a percentage whereas the number you get when monitoring at home is a numeric value (mg/dL or mmol/L).
QUICK ANSWER: A1c is an average measure of glucose in your bloodstream from the previous 3 month period. The normal range is between 4-6% but your individual goal may be set higher initially or long term, depending on a few factors – keep reading to learn more.
My blood readings range 5-7 (90-126), always. I understand that but so often the literature talks about your A1C readings. How do I get that and what is it?
The HbA1c is a percentage whereas the value you get with daily testing is a number expressed in mmol/L or mg/dL.
Your daily levels change on an ongoing basis whereas A1c provides a 3 month average.
A1c/ Blood Sugar Conversation Table
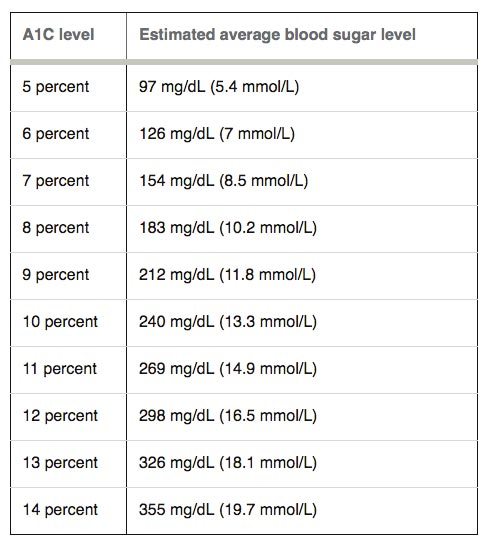
For example, if your A1c is 6%, your blood sugar has been running 7 mmol/L or 126 mg/dL on average.
Both numbers are important as an indicator of blood sugar control. But one important thing to point out is we can’t make the reverse assumption. For example, you can’t look at the daily reading of 7 (126) and assume your A1c is 6% because you only know what your glucose level is the time you check it, not as it fluctuates throughout the day or overnight.
An A1c test must be performed at a physician’s office or lab. If you don’t know your A1c, schedule an appointment with your doctor to have it drawn or call to request it.
QUICK ANSWER: Your A1c is a blood test measurement that is ordered by a physician 1-4 times per year. It is an indicator of blood glucose control.
I’m approaching borderline of A1C. I’ve already lost 30 lbs (13.6 kg). Would losing the additional 40 lbs (18 kg) be enough to remedy the A1C levels?
While there are no guarantees, if you have 40 pounds to lose to approach a healthy weight range, the only way we’ll know is if you do it!
If it doesn’t improve A1c (which would be surprising as I highly suspect it will), worst case scenario is you end up feeling better, looking better and with a better A1c than had you not lost the 40 pounds.
Unfortunately, there are many factors that impact A1c, some of which are controllable and some of which are not. Weight is a big one, but not the only one. For instance, your diet, your level of insulin resistance, the amount of exercise you do, and other factors – can all influence A1c levels.
QUICK ANSWER: Weight loss can help lower A1c but it’s not the only factor – diet, lifestyle, insulin resistance and other factors may also influence your numbers.
What is the quickest way to lower my A1c without using prescription drugs or insulin by diet changes?
That’s a great question and pretty much the essence of our site here at Diabetes Meal Plans!
The quickest and best way to lower your A1c is through your diet – what you eat on an everyday basis; and lifestyle changes.
I’d encourage you to check out this link to our top 10 essentials, including diet guidelines, healthy foods, explanation on carbs and amounts, and much more – including a plethora of recipes to help you get started!
QUICK ANSWER: The quickest and best way to lower your A1c is through your diet – what you eat on an everyday basis; and lifestyle changes.
What type of things can I do to keep the A1C going south and what is a good number to hit?
Weight loss if overweight, following a healthy carb-controlled diet (see above for links), managing stress, sleeping well, and taking medication if needed, are all key to reducing your A1c.
As far as your number goal is concerned, that should be individualized between you and your doctor based on a lot of factors such as how long you’ve had diabetes, what your current control is, your age, whether you are taking insulin, and so forth.
A great goal would be less than 6.5% (under diabetic range) and if you can reduce it to under 5.7%, that would put you even out of pre-diabetes range.
However, for most people who have had diabetes for any significant length of time, 7% may be a more realistic goal to help minimize complications.
That said, those who have had poorly controlled or brittle diabetes for many years, the elderly, and those taking insulin may have a more liberal goal like 8%, simply because they may not be able to realistically achieve a lower goal without risking hypogylcemia.
QUICK ANSWER: Diet is one of the best ways to lower A1c. Although a normal A1c range is 4-6%, your individual A1c goal should be decided with your physician because it can be dependent on a few different factors.
Q: A1c readings. Can you figure this on your own beside the doctor doing it?
No, you can’t figure this out on your own. To know your HbA1c accurately, you need to have that particular blood test run by a lab and it has to be ordered by a physician. It cannot be performed on a home meter. It is a test done 1-4 times per year in those with, or at risk for diabetes.
QUICK ANSWER: You can’t figure out an A1c measurement on your own. It is a blood test ordered by a physician.

I want to get myself off Metformin ASAP. If my A1C drops from 7.4 by a couple points, do you think I should have to continue taking Metformin?
That is completely between you and your ordering physician. I would question why you want to get off of metformin asap.
If you are having symptoms like diarrhea, you may want to discuss trying a different medication. If you aren’t experiencing symptoms, I would encourage you to discuss your concerns with your doctor.
In terms of medications, metformin is a generally a safe and effective medication and helps the body put less sugar out into the bloodstream.
In saying that, if your A1c drops a couple of points (ie: from 7.4 to 5.4), there would likely be no need to take metformin as you would be out of even pre-diabetes range. However, if you mean fractions of points like 7.4 to 7.2, you are still out of goal range and at risk for diabetic complications.
QUICK ANSWER: If you can lower your A1c within normal range, there would be no need to take metformin.
My A1c is 10 now. I am always craving to eat sugar. I can’t control sugar eating. Please help.
Ten percent is very concerning for an A1c. It indicates your blood sugar levels have been running 240 (13 mmol/L) on average.
This puts you at pretty high risk for diabetic complications. Ideally, you need to be aiming for 7% or less as a good initial goal.
Sugar cravings can be very challenging. We have a great article here with some tips and ideas.
You’ll also be surprised that as your levels lower and you gain better control, your cravings will reduce as well.
If you truly feel way out of control, you may consider getting professional help by way of counseling. Everyone experiences cravings, but true addictions are a bit more difficult and something you may not be able to battle alone.
QUICK ANSWER: Dealing with cravings can be a challenge but a high A1c level puts you at substantial risk of complications. Therefore, it’s worth managing cravings and getting your levels lower.
If you have A1c questions of your own, please leave them below and I’ll do my best to answer them.
Please pin, tweet or share this post. Thanks!


Patti Ashton
I just had my A1 c done. I was at 6.1, now it’s 5.3. I know that is out of pre-diabetic range. But my morning BS are in the high 90’s, up to 106 some mornings. So is this still considered pre-diabetic? I’m still closely watching my diet.
Thanks,
Patti
Carol L Johnson
I have been on high doses of steroids for over one year, but have been slowing tapering down. My weight has increased by 30 lbs in the last year and my A1c has increased to 9.5. My doctors have been telling me that I shouldn’t worry about it too much because the A1c will improve when the hydrocortisone is reduced. However, I now have tingling in my feet, I am very fatigued, and I am feeling weak and have frequent sweating. I am also struggling with poorly functioning adrenals. I have been taking my morning blood sugars and they are running between 150-180, however I’m shocked that after I eat breakfast of 2 eggs and lightly butter toast that my blood sugars are running 260-270. I am really scared about this. Should I seek further help with my diet?
Elizabeth
If it were me, I would seek further medical help. Regardless of the reason (whether from lifestyle, genetics, age, steroids, etc), high blood sugar is increasing your risk of complications and clearly you are experiencing that. You need to find a doctor who can help you manage your blood sugars through medication (oral or injection) to get them back under control in addition to watching your diet. Cutting out the toast is not going to bring your sugar down as much as it needs to come, it seems the problem is the steriods–if they must be continued, you need something to counter their effects.
Jeanette Molczan
I have a question that I hope you can give me an answer to. I have 2 Glucose Meters, each from different companies. I regularly just use one company of meter but if I’m not satisfied with the results, I will use the other one, too. It seems that the 2 have different results with 1 being at least 10-15 points lower. Why the difference and which one is accurate?
Thanks,
Jeanette
Elizabeth
Home glucose meters are not intended to be 100% accurate (that’s why we can get them really cheap) and there can be up to a 20 point variance per FDA regulation. That means that if your blood sugar is 100, your meter can read “110” or “90” and still be considered accurate. One of your meters simply runs a bit higher than the other. Use a calibrating solution (see above comment) to test and ensure accuracy on both!
Rosemary
Hi, I was diagnosed just over 2 months ago with type 2. My level was 29 and now after losing 11 kg and meds it is in normal range. I lost some of my eye sight but over all I feel good. I read on diabetic web sites that people who lose weight and live a healthy lifestyle can stop all meds and no longer considered to be diabetic. My question is, my doctor is adamant that I will be insulin dependent and my diabetes will get worst, is that right? If so, what can I do to turn it around.
Elizabeth
Nice job with the weight loss and improvement Rosemary! So glad you’re feeling better. What we know is that diabetes is a progressive condition–that is it will not simply ‘go away’ because it is a combination of depleted pancreatic function and insulin desensitization. Diet, exercise, weight loss and medications can all help to improve outcomes and delay need for insulin, sometimes indefinitely. Some people do see a bit of “regression” with these changes–however they still have diabetes, it’s just considered “controlled” at that point. It is not necessarily the case that you will be insulin dependent and whether your diabetes gets ‘worse’ depends on how well you keep your numbers under control. The better controlled they are (diet, exercise, medication, weight loss, etc) the fewer complications!
Lori
I have a question. I take my levels in the morning. I take it on one hand and its 1 number, then I take it on the other hand within 1-2 min. because i feel the first one wasn’t accurate–and the 2nd one is 40-50 points LOWER. How can that be? Has happened 2x this week. I just started doing this because I wasn’t getting the numbers I expected being on a low-carb diet for over 3 months. I’m 70, and weigh 235 (just lost 20 lbs, and going)
Elizabeth
I would calibrate your meter. If it were 5-10 points, maybe even 20 I’d say it could just be inaccuracy or the fluctuation of glucose, but that is way too big of a difference. There should be a calibrating solution with your machine and if not you can pick one up from the pharmacy. You may also want to consider getting a new meter–sometimes they are faulty or don’t work as long after a while.
Bruno
I have lost 27 kg in 5 month.
MY blood sugar readings are from 80-110 fasting and postprandial.
My A1c on 8 May 17 was 5.3 about 3 month from my mild stroke.
I was on diabetes medication glumet and velmetia since stroke.
I am still taking 2 tablets 500mg metformin per day.
If I reduce or stop metformin in the future what will happen?
Elizabeth
Hi Bruno–it’s impossible to know with certainty because we don’t know the extent of the role it is playing. I would discuss it with your doctor and maybe consider a trial of weaning from them and see if your control remains good–if not, it’s still a great medication many people can be on long term with little to no side effects
.
Sandy
I have been a type 2 diabetic for 25 years. In the beginning i followed the ADA recommend diet. I felt deprived and my A1C was 7.8 even with meds. I was gaining weight. When my weight hit 247 i changed direction. Read Atkins and became an RN. Slowly began elimiating carbs. Now keep carbs to 50 or so a day. My weight is 135. Ok for 5’4″. A1C is 6.5 and use very little oral meds for control. Don’t feel deprived and don’t count calories. I encourage everyone to carb count for a better life!
Jedha
Awesome results Sandy!! Lower carb is the only way to go, that’s why we try to educate people about it here.
Amy
Great job, Sandy! My daily blood sugars remain steady due to counting carbs. I eat 3 small-medium meals per day and 3 small, nutritious snacks to blood sugars steady. I also exercise a lot. The gym is my other home! I have had no issues counting carbs & eating protein with each meal/snack.