Poor diabetes control can come with a host of medical complications, ranging from the uncomfortable to the life-threatening.
Keep reading to learn what those complications are, and more importantly, how to prevent them.
What is Poor Glycemic Control?
When you have blood sugar levels that are consistently outside of the “normal” range, you are experiencing poor glycemic control (or poor diabetes control).
Chronically elevated blood sugar levels commonly occur in people with type 2 diabetes who don’t treat their condition holistically; medication alone is often not enough to get blood sugar levels stable over the long term!
Healthy lifestyle changes are a vital part of tackling diabetes, getting blood sugar levels within a normal range, and avoiding some of the nasty complications of poor glycemic control.
So, what counts as “normal” anyway?
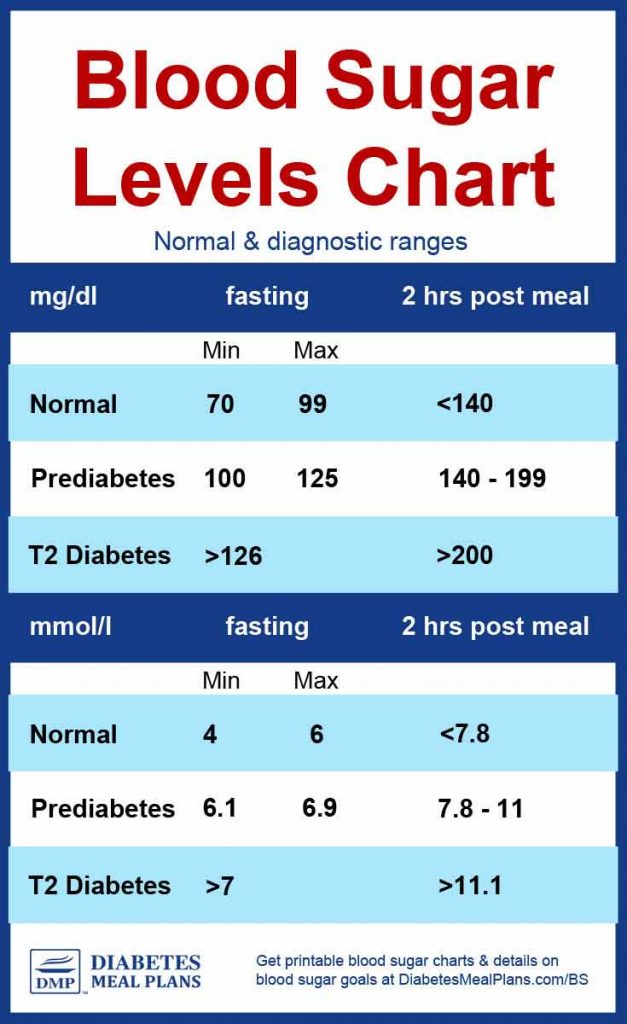
The chart below shows two different measurements of blood sugar control: fasting blood sugar (taken in the AM before food or drink) and post-meal blood sugar.
You could fall into the category for normal, pre-diabetic category, or type 2 diabetic blood sugar levels.
People with uncontrolled diabetes can having blood sugar levels well beyond those shown on the chart; as your levels get further out of range, your risk for diabetes complications rises.
Where do your blood sugar levels fit?
Another good measurement of your overall blood sugar stability is the HbA1c blood test which represents an average of blood sugar levels over the past 3 months.
An A1c of over 7.0 indicates uncontrolled diabetes with elevated glucose levels.
| HbA1c Levels | |
|---|---|
| Normal | Below 5.7% |
| Prediabetes/Controlled Diabetes | 5.7% to 6.4% |
| Controlled Diabetes | 6.0% to 6.9% |
| Uncontrolled Diabetes | 7.0 and above |
Symptoms of Poorly Controlled Diabetes
One of the tricky things about diabetes is that you may have few or no observable symptoms until your blood sugar levels are extremely high for an extended period of time.
Although spikes of high blood sugar can make you feel sleepy or groggy for a while, you typically won’t “feel” high blood sugar levels themselves…but you will be able to feel the downstream consequences once blood flow becomes impeded and chronic inflammation takes over.
This is why it’s important to self-test blood sugar often and get an A1c test at the doctor’s office so you know where you’re at before complications arise.
The complications of diabetes can get very serious but you don’t want to wait until that point to start treating it!
Complications of Poorly Controlled Diabetes
Cardiovascular Disease
The blood vessels of the body, heart, and brain are vulnerable to inflammation and damage caused by elevated blood sugar levels. The nerves that supply the heart are also sensitive to these changes.
Add in some common comorbidities like high triglycerides and high blood pressure, and you’ve got a recipe for cardiovascular disease. That means heart attacks, strokes, atherosclerosis (clogged arteries), edema (swelling), and congestive heart failure could all be on the table.
Sadly, cardiovascular disease is the leading cause of death in multiple Western countries…with 2/3 of people with diabetes dying as a result of it.
The symptoms of an impending heart attack or stroke may be subtle; sometimes there are no direct warning signs at all. This is why being in the know about your current blood sugar levels and actively working to lower elevated levels is so important.
However, the havoc caused by poor blood circulation and blood vessel inflammation doesn’t just stop at the heart.
Retinopathy
The blood vessels in the back of the eyes are extremely delicate and vulnerable to damage caused by high blood sugar levels.
Damage to these blood vessels (called retinopathy) can slowly develop over time or come on rapidly in some cases. Either way, retinopathy can develop into blindness if left unaddressed.
People with type 2 diabetes are also at higher risk for cataracts and glaucoma, so it’s important to get screened for these conditions by an ophthalmologist, annually.
Nephropathy
The kidneys are another set of organs which are loaded with tiny, fragile blood vessels that are susceptible to damage from high blood sugar levels. Nephropathy (not to be confused with neuropathy, which is generalized nerve dysfunction).
The kidneys work round-the-clock to filter and excrete excess glucose. Over time, exposure to higher-than-normal glucose levels damage the vasculature, leading to nephropathy.
While kidney damage is a very slow, gradual process, it can turn into a life-altering condition called kidney failure (stage 5 kidney disease) in which a person’s kidneys have ceased functioning and they rely on dialysis to stay alive.
Dialysis usually requires the patient to visit a center (often 3 days every week) and connect to a machine that filters waste products from your blood.
Neuropathy
Nerve damage (neuropathy) is a very common complication of uncontrolled diabetes. Excess glucose in the blood can damage the capillaries that supply nerves all over the body, resulting in chronic nerve pain, tingling, numbness, and loss of sensation that can result in injury.
Peripheral neuropathy typically starts in the feet and hands, moving up to the arms and legs. Neuropathy can also cause sexual dysfunction in both men and women.
Chronic neuropathy and circulation issues can especially impact the feet, causing cuts and sores to heal slowly and poorly.
In extreme cases, amputations of the toes or foot may be necessary.
Infections
People with diabetes often have impaired immune function. This can lead to more infections both systemically (like the flu) and locally (like ulcerated feet or an infected tooth).
It’s vital to stay on top of systemic infections by getting all the vaccinations recommended by your doctor and also maintaining basic health habits like good sleep, well-rounded nutrition, and stress management.
To prevent and address local infections, visit your dentist twice a year for a cleaning and check-up. Your dentist will examine your mouth for any signs of gum disease, fungal infections, or infected teeth.
To maintain your feet at a basic level, check them daily for cuts, blisters, and abrasions. To go the extra mile, have your feet checked by your doctor at every office visit and schedule a yearly visit with a podiatrist to keep everything in tip-top shape.
Poor Mental Health
Mental health issues like depression and anxiety are already more common among people who have diabetes, but uncontrolled blood sugar levels can make things worse.
While it’s normal to feel anxious, stressed, or down during certain periods of life, talk to your doctor if you experience signs of clinical depression or anxiety that are causing dysfunction or significant destress.
Research also suggests that there could be connections between diabetes, insulin resistance, and conditions of cognitive decline such as Alzheimer’s.
Besides talking to your doctor about mental health or cognitive concerns, the best thing you can do to give yourself a leg-up is to practice good health habits in all areas of diet and lifestyle.
So now, let’s get to the good part!
How to Reduce Your Risk for Complications
This article isn’t meant as a fearmongering thing, but as a message of hope – these complications don’t have to affect all people with type 2 diabetes.
Diet and lifestyle changes (along with medication if necessary) can make a world of difference, from stabilizing blood sugar levels to lowering A1c, to boosting your energy and reducing chronic pain.
This is something to be excited about…you can take steps toward better health today!
An amazing statistic: Just a 1% reduction in A1c is associated with a:
- 21% reduction in diabetes-related death
- 14% reduction in heart attacks
- 37% reduction in microvascular complications
Such a small change in A1c can have a massive impact on your overall health and quality of life. Just imagine how great things would be if an elevated A1c was brought all the way into a healthy range!
Not sure how to lower your blood sugar and A1c through diet?
Here are some helpful resources to kick-start your healthy, low carb lifestyle:
- Dieting for Better Blood Sugar (learn the basics on nutrition and healthy eating)
- Type 2 Diabetes Low Carb Diet Guidelines (find out what eating “low carb” actually means)
- Diabetes Friendly Food List (a convenient master list of low carb foods)
- 5 Steps To Putting A Low Carb Diabetic Diet Into Practice (a no-nonsense guide to get you started)

Barbara
It’s not showing up on my email
Trevor Barnes
Very informative.
Thanks
Shirley Clark
I have been struggling for several years, what has been most helpful for me is tracking my blood sugar after every meal or snack. Knowing what foods elevate my blood sugar. If I eat carbs it’s in the morning only, like a small red potato or half of an English muffin. Then I’ll have a snack , 1 Oz unsalted cashews or a Spinach Celery flex seed cap of alo-vera juice, cap of beet juice a slice of lemon bottle water in a blender. That will bring my blood sugar down at least 50 points. Then lunch no carbs then dinner no carbs. My Fasting number is 200 by the end of the day my number is 140 and below. I TAKE NO MEDICATION. I continue to work The Fasting number, I go to bed with a 145 and wake up with 200. My last A1c was 7. I’m working on bring that down to 6.5 or lower.