Table of Contents[Hide][Show]
Scenario #2: High Blood Glucose+−
- Example#1: My husbands blood glucose is around 220 (12.2), is this high?
- Example #2: Daily glucose readings have been getting into the high 200s (11s) but the A1C test has dropped from 6.4 to 6.2. Bedtime readings around 100 (5.6) and mornings 150+ (8.3+). I don’t understand any of these numbers. Can you help?
- What is A1c and what numbers for percentage indicate a healthy range?
- Why It Helps to Log Your Numbers
Since the inception of our website, we’ve received hundreds of personal questions, many of them asking about a specific blood glucose measurement and how to interpret it.
We LOVE this because it means people are being proactive in their diabetes management, making efforts to educate themselves and taking an active role in their health!
While we’ve written more extensively about healthy blood sugar ranges here, listed a detailed blood sugar levels chart here and described the links between home glucose checks and A1c here, today we’re here to look at some practical examples of the numbers you might see and how to interpret them.
*Please note that the following scenarios are simply describing general case-scenarios without a full assessment of all the information. Your individual treatment plan should take into consideration your current health, disease history, risk factors, age, physicality, capabilities, preferences and your willingness to prioritize diabetes management.

Scenario #1: Fasting Blood Glucose
Example#1: My fasting numbers are 101-118 (5.6-6.6), does this sit within range?
This is a fairly good range. The optimal range is 70-100 (3.9-5.5), which is considered ‘normal.’ So if you are coming in the range of 101-118 (5.6-6.6), this is close.
For people with type 2 diabetes, having elevated morning blood sugar levels is quite common. Metabolism, hormones and various other factors can change in diabetes, all of which influence fasting levels. The best course of action is to get your daily blood sugar levels within a healthy range, and keep them there, as this will also influence your fasting numbers.
In terms of fasting glucose and risk of complications, we do need more data. However, studies show that a fasting level under 121 mg/dL (6.7 mmol/l) have the least amount of risk for acquiring some vascular diabetic complications such as retinopathy and nephropathy. Other studies suggest fasting levels over 126 mg/dL (7 mmol/l) is where diabetic complications begin to increase.
Overall your goal is to try to get your fasting levels as close to normal as possible. At this point, with levels of 101-118 (5.6-6.6) it sounds like you’re doing a pretty good job overall, so keep working on it!
Example #2: My fasting numbers are inconsistent, one day it’s 133 (7.4), the next it’s 171 (9.5). Are these numbers good or bad?
Both levels aren’t ideal. 133 (7.4) is a bit higher than optimal, but not terribly out of range, whereas 171 (9.5) is concerning. Above 130 (7.2), risk for complications starts increasing.
One of the best strategies to improve fasting levels is moderate exercise daily. This improves overall insulin sensitivity when done regularly and consistently. I would check your meter with a calibrating solution to see if it’s accurate, and if so, start keeping track of other factors such as how many carbs you’re eating, meal timing and what specific foods you are eating each day to detect patterns.
Also, if you sleep very poorly, your hormones have not been appropriately restored and will not work the best. This can often be a reason for high fasting levels.
Example #3: Fasting 93.6 (5.2) is this number a problem with T2?
No, it’s not a problem. You’re in the clear–nice job!
Remember that the goal is patterns rather than individual numbers, so check it as frequently as you and your doctor agree but be sure you are in this healthy range regularly before getting too excited.
Also, if your A1c is not reflective of a healthy range, it may be indicative that, while fasting levels are great, your daytime readings (after meals) are higher than you’d like.
For example, if your A1c is 7, this means you have an average glucose of 154 (8.5). Then it’s smart to check after meals to see when it’s running higher.
Scenario #2: High Blood Glucose
Example#1: My husbands blood glucose is around 220 (12.2), is this high?
This is too high by any standards. Even the most liberal standards would draw the cutoff at 180 (10.0).
However, if this is a recent diagnosis and he’s just starting to make changes, it may take some time to bring down. If it remains this way for more than 1 month, his diet, lifestyle or medication should be adjusted to help get the numbers down.
Reducing the total carb load (if it’s high), changing the types of carbs at meals (from white/refined grains or sugar to vegetables, and other higher fiber whole foods – try adding chia seeds!), exercising daily, losing weight if obese, and reducing stress, are all natural lifestyle changes that can help improve readings reducing the amount of medicine needed.
Example #2: Daily glucose readings have been getting into the high 200s (11s) but the A1C test has dropped from 6.4 to 6.2. Bedtime readings around 100 (5.6) and mornings 150+ (8.3+). I don’t understand any of these numbers. Can you help?
Sometimes readings can feel all over the place, which indicates a need to adjust diet, lifestyle or medications, recalibrate your meter, or both.
An A1c of 6.4-6.3 translates to an average reading in the 130s (7.2-7.8).
If your home meters shows 150 (8.3) in the morning (a bit high) and in the 200s/11s (not sure when, after meals?) and 100 (5.6) in the evenings (a bit low right before bed) it means your meter is off, or you are dropping low in the middle of the night or some other time you aren’t aware of.
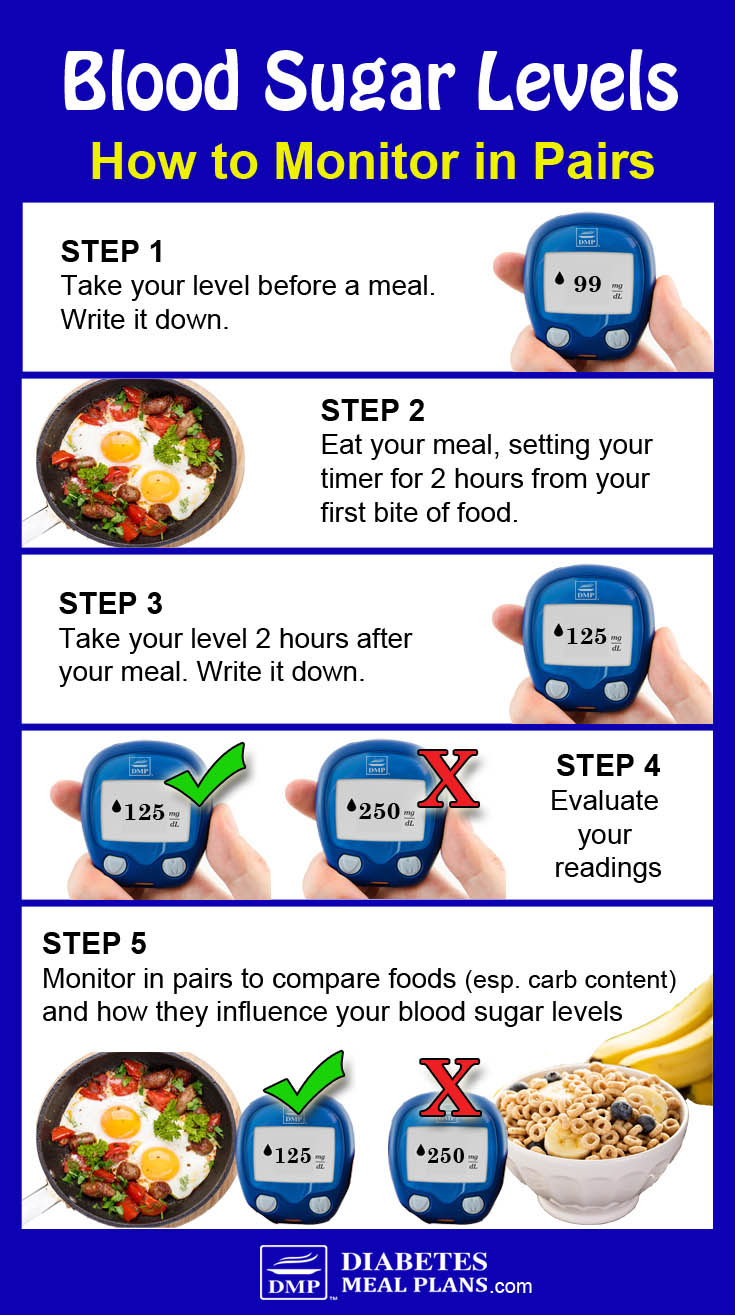
First step: calibrate your meter with the control solution it came with. If it is accurate, keep a detailed log of readings before and after meals (2 hours) as well as what you ate. This is called testing in pairs–if the number is more than 40 points different, the meal had too many carbs or more insulin is needed to help cover them.
If taking insulin, the amount and timing may need to be adjusted to help you with your overnight or daytime levels (do not make any changes without your physician’s order). If a person is taking insulin, through a bit of trial and error (per your ordering physician’s recommendations), you can easily achieve better control.
Scenario #3: Prediabetes
Example #1: What is normal for prediabetic when you wake up in the morning … before you eat anything?
Anything under 100 (5.5) is great! 100 (some say 110)-126 (7.0) is considered ‘pre-diabetes’ range.
If your fasting levels are higher than this, you may have undiagnosed diabetes and should schedule an appointment with your doctor to discuss a treatment plan.
Example #2: In the meter reading my fasting rating was 100 (5.6) so I wanted to know if I have prediabetes?
100 is right on the cusp!
Remember that meters can be off by as many as 20 points (mg/dL) and still be considered accurate, so if this was only one time and doesn’t happen again, you’re probably fine. Your meter may have just run a bit high.
However, if you are seeing these numbers consistently, you probably have pre-diabetes. This is a great spot to be in because you still have the potential to ward off a full diagnosis of diabetes through lifestyle changes!
If you have already been diagnosed with diabetes and you are seeing numbers in this range, that’s AMAZING–great job improving your control!
While diagnostically, you wouldn’t be classified as ‘pre-diabetes’ but rather ‘controlled diabetes,’ your hormones and blood glucose control is equivocal to that of prediabetes. Complications are minimized or absent in this range.
Scenario #4: Healthy Blood Sugar Ranges
Example#1: What should blood sugar be during the day? What numbers should I look for?
We have a great chart available here, but in short, fasting ranges under 110 (6.1) are awesome and under 130 (7.2) are still pretty good.
Post-meal (2 hours after eating) readings under 140 (7.8) are awesome and under 180 (10.0) are still acceptable.
Avoid checking immediately after a meal as this has not yet allowed sufficient time for insulin to have brought glucose within the established ranges. The best time to check is two hours after a meal.
Example #2: Why does everyone have a different answer on what the right blood sugar range is?
This can be confusing but there are good reasons for it. Different organizations and doctors will have different expectations for different people based on different goals. The reason for this is all individuals are different (hence the need for a ‘range’) and their goals should be individualized based on many factors specific to them, not generally to the whole population.
People who have had diabetes for many years, are on a lot of insulin or elderly will have much more liberal goals because tighter control may result in poorer quality of life.
On the flip side, someone who is younger, on fewer medications and more recently diagnosed has a lot better shot at getting tight control early on and so avoid longer term complications.
Overall though, keeping blood sugar levels under 140 mg/dL or 7.8 mmol/l two hours post meal, is a globally accepted optimal healthy range.
What is A1c and what numbers for percentage indicate a healthy range?
A1c, or Hemoglobin A1c, is a percentage of glycated (stuck with sugar) red blood cells in a given person at the time of a blood draw. Because red blood cells turn over every 3 months, this provides a nice 3 month average of how blood sugar levels have been running.
However, it does not capture day to day variation. For example, if your A1c is 7, your sugars have been running 154 (8.5) on average. It does not tell you when blood sugars are problematic (ie. in the mornings, after meals, before bed, overnight etc).
A1c of <5.7 is considered normal (or <6 in some regions of the world), 5.7-6.4 is pre-diabetes (6-6.4 in some regions of the world) and above 6.5 is diabetic range. Generally, if a person with diabetes keeps their A1c under 7, that’s a great goal. If you are able to knock it under 6 that would be optimal.
Why It Helps to Log Your Numbers
Remember to write those numbers down in a log, diary or app.
The purpose of home glucose monitoring is to learn how different variables (food, medicine, exercise, sleep etc) affect your blood sugars so as to make informed decisions based on the trends and patterns you see.
It’s always a good idea to log additional information such as any symptoms you might have and other patterns of behavior like exercise, carbs eaten, stress levels, and sleep quality.
The more you track what is going on, the more you’ll be able to make associations with what causes your blood sugar to go high or low.
Hope you found this info on blood glucose measurement helpful. If you have questions of your own, please feel free to leave them below.
Need help to lower your blood sugar? Join us as a member today.


Guni
this was very helpful and so well explained, thank you!
jim
Are meters actually recalibrated or do you replace them if they go out of calibration?
Jedha: Nutritionist (MNutr)
Overall it depends on the brand of meter. Some meters come with a calibration solution; otherwise this should be available at most drug stores. You can check with the pharmacist or contact support of the brand of meter you have. And of course, sometimes meters will have to be replaced.
Wayba
This is a great article, informative! There was one part that mentioned calibrating the monitor if we think it might be incorrect. How is that done?
Since changing my diet, my numbers have gotten lower, but I’ll be checking in for sure with my blood work at the end of September.
Emily - Dietitian (MS, RD)
Some meters come with a calibration solution; otherwise this should be available at most drug stores. I would verify with your blood work and if there seems to be a discrepancy then you’ll definitely want to follow up with the calibration solution and let your doctor know.