Table of Contents[Hide][Show]
- LISTEN TO THE PODCAST
- CHAPTERS
- Overview
- What Is a Good Fasting Blood Sugar?
- When to Test Fasting Blood Sugar
- Why Does Fasting Blood Sugar Fluctuate?
- Try a Fiber Boost at Night
- What About Exercise and Fasting Blood Sugar?
- The Dawn Phenomenon and Morning Spikes
- High Morning Numbers and A1c
- Could It Be LADA, Not Type 2 Diabetes?
- Transcript
If you’ve ever wondered why your blood sugar is higher in the morning—even if you didn’t eat anything—you’re not alone.
Fasting blood sugar, or morning blood sugar, is one of the most common frustrations for people with type 2 diabetes and prediabetes.
This episode answers your questions about fasting glucose levels and shared practical tips that can help you bring those numbers down naturally.
LISTEN TO THE PODCAST
CHAPTERS
2:00 Optimal fasting blood sugar ranges
3:11 When is the best time to take a fasting measure of blood sugar?
4:17 Why are my fasting blood sugar levels fluctuating?
5:56 Does fiber at night lower fasting levels?
7:20 Does morning exercise impact my fasting blood sugar levels?
10:16 Why is my fasting level high when I haven’t eaten any food?
12:26 How can I lower my fasting blood glucose level?
14:58 Extremely high fasting levels and numbers
Grab Your Free Copy To Lower Fasting Blood Sugar Levels
A mini e-guide with Scientifically Proven Strategies that actually work!
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
Overview
Here’s a recap of the key insights—along with steps you can take to improve your own results.
What Is a Good Fasting Blood Sugar?
Let’s start by defining the target ranges:
- Optimal (normal): 70–99 mg/dL (4–6.0 mmol/L)
- Still good: up to 110 mg/dL (6.1 mmol/L)
- Realistic goal: under 130 mg/dL (7.2 mmol/L) if you’re just getting started
Your personal goal is to move toward the normal range—or at least as close to it as possible. If you’re consistently above that, there’s plenty you can do to help.
When to Test Fasting Blood Sugar
A common question I get asked is: When is the best time to take a fasting blood sugar test?
The answer is simple: right after waking up, before you eat or drink anything—even before your coffee.
Making this part of your morning routine can really help track progress over time. Try storing your glucose monitor where it’s easy to access, like beside your bed or in the bathroom.
Why Does Fasting Blood Sugar Fluctuate?
Even if you’re eating well, your numbers can still vary. Blood sugar fluctuations are completely normal.
For example, Betty shared her fasting blood sugar ranges from the mid-90s up to 116 mg/dL (5.0–6.4 mmol/L).
While she felt frustrated, these numbers are not far off from the goal. If you’re in this range, it usually means you’re on the right path, and a few small tweaks might help you improve further.

Try a Fiber Boost at Night
Michael asked if eating more fiber at night could help with fasting glucose.
The answer is yes—especially soluble fiber. A supplement like psyllium husk taken before dinner may help improve insulin sensitivity and slow glucose release.
In fact, studies show that psyllium can lower fasting blood sugar by up to 50 mg/dL (2.9 mmol/L) after 8 weeks of consistent use.
Try this: Mix 5g of psyllium husk into 250 ml (about 1 cup) of water, 20–30 minutes before your evening meal.
What About Exercise and Fasting Blood Sugar?
If you exercise in the morning, like Hanah who swims 2 km (1.2 miles) most days, you might see a temporary spike in your blood sugar after your workout. This happens because your liver releases stored glucose to fuel your muscles—a totally normal response.
Key tip: If you’re doing a lab fasting blood test, do it before you exercise so the reading reflects your true fasting level.
The Dawn Phenomenon and Morning Spikes
Several listeners, including Susan and Francinah, noticed that their fasting blood sugar was sometimes fine—and sometimes frustratingly high. This can be due to:
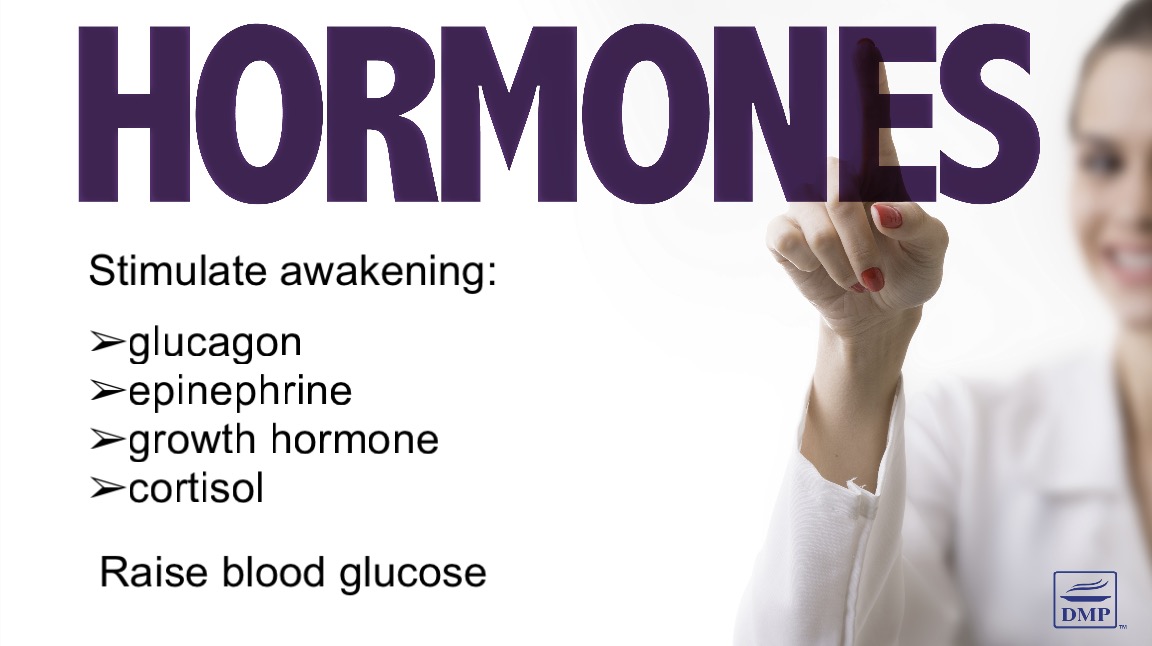
- The dawn phenomenon: A natural hormone-driven release of glucose before you wake
- The feet-on-the-floor effect: Simply getting out of bed and moving around can spike glucose
What can help?
- Try eating a small protein– or fat-based snack first thing (e.g., a handful of nuts)
- Avoid doing chores before breakfast
- Choose a low carb, high-protein breakfast
- Refer to the strategies shared in Episode 38 for more ideas
High Morning Numbers and A1c
If your morning numbers are always high—like Francinah’s 8–10.5 mmol/L (144–189 mg/dL)—it could be tied to overall elevated A1c or post-meal spikes from the day before.
Getting your A1c into a healthy range (ideally under 6%) is the first step, and that often means reassessing your daily nutrition strategy.
Could It Be LADA, Not Type 2 Diabetes?
One important case was Rebecca, who had high fasting numbers, rapid A1c increase, unexplained weight loss, and what seemed like healthy habits.
If this sounds familiar to you, it’s worth asking your doctor about LADA (Latent Autoimmune Diabetes in Adults)—sometimes called type 1.5 diabetes.
Tests to ask for:
- C-peptide
- GAD antibodies
These help distinguish whether your body is no longer producing insulin, which would require a different treatment approach.
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful people, Dr Jedha here and thanks for joining me for an episode answering questions about morning blood sugar levels, otherwise known as fasting blood sugar levels.
Before we dig into this discussion, I want to let our members know that we now have a new healthmap available that focuses specifically on how to lower fasting blood sugar, with a step-by-step strategy to help you focus on the right strategies and of course how to lower fasting blood sugar naturally so we walk through primary nutrition strategies and proven natural supplements, along with other science-backed ways you can get those morning numbers lower. So for our members, just head to the members site and in the Guides you will find this new healthmap of lowering fasting blood sugar.
02:00
Before we dive into today’s questions, let’s just do a recap on fasting blood sugar levels – the numbers.
The goal ranges do vary slightly depending on the recommending agency, but generally you’ll see these ranges:
The optimal normal range is between 70-99 mg/dL or 4-6 mmol/l. Your goal with pre or T2diabetes is to try to get into this normal range or as close to this normal range as possible. For type 2 diabetes, fasting levels of 110 or 6.1 is still considered good. And then up to 130 or 7.2 is a more liberal target range, but it’s realistic for many people, especially at first. But again, ideally you want to be aiming for under 100 or under 6.
So now that we’ve got those numbers straight, let’s explore some questions regarding fasting blood glucose levels.
03:11
Brad asked: When is the best time to take a fasting measure of blood sugar?
Now, I know for some of you this might seem a simple question but those newly diagnosed often have questions and there is no stupid question, except the one you don’t ask!
Brad, it’s best to test your blood sugar right when you get up and that’s what makes a fasting blood sugar test a highly convenient test for many people. If you make it part of your morning routine, such as after you go to the bathroom in the morning, it’s easier to remember. Keeping your supplies by your nightstand or in the bathroom or kitchen–wherever you are most likely to remember–will help facilitate this routine. And obviously making a note of that in a notebook or onsite log such as we provide to our members, so you have a record of those numbers and patterns, that’s important. But yep, it’s literally the first thing in the morning that you want to be taking a fasting measure of blood sugar.
04:17
Betty said: My fasting blood sugar ranges from the mid 90’s to anywhere from 104 to 116. It’s so frustrating. I’m trying to be very careful what I eat and drink.
For our metric listeners, those numbers are between 5.0 and 6.4. So Betty, while you may feel frustrated it’s normal to see some fluctuations, a morning number or any other blood glucose number is never going to be exactly the same each day. A fasting blood sugar in the 90s to low 100s is actually not too bad. If you have some days at 90 (5.0) your numbers are sometimes in the normal range, exactly where you want them. And on some days your numbers are going marginally above normal 116 or 6.4, so overall you say you are very careful with what you eat and drink and the numbers provide a pretty good sign you’re on the right track. If you’re aiming to bring it lower, a few key factors can help: meal timing (especially your evening meal), protein and fat balance, managing stress and sleep, and using natural supplements, berberine being one good example which we covered extensively in episode 21. Since you’re within the normal range or just outside it, making a few tweaks to your routine will likely be enough to get those numbers down a little lower, and you can find more tips on doing this in episode 38.
05:56
Michael asked: Should I increase fiber intake possibly at night and would it help lower my numbers in the morning?
Great question, Michael! A fiber-rich evening meal may help with morning blood sugar, but its impact varies from person to person. Research shows that soluble fiber, for example, taking a fiber supplement like psyllium can slow glucose absorption and improve insulin sensitivity over time and is very beneficial for lowering fasting blood sugar levels. In fact, studies have shown that after 8 weeks of supplementing with psyllium, fasting blood sugar reduces by an average of 43 to 52.6 mg/dl (2.4 to 2.9 mmol/l), by anyone’s measure that’s a substantial reduction. So in addition to eating a fiber-rich meal, try taking 5 grams of psyllium husks in at least 8-ounce (250ml) of water 20-30 minutes before your evening meal. We’ll also leave some more info on psyllium in the show notes and for members, you can find all the details on the most effective supplements for fasting blood sugar all listed in the new healthmap on lowering morning blood sugar, which can be found in your guides.
07:20
Hanah said: I swim 2 kilometres (1.2 miles) every morning, 6 days a week. I have taken blood sugar readings on waking and it’s around 6.2 (111). When I return from swimming the reading is 6.8 (122). Why? Most waking hours my blood sugar is between 4.0-6.0 (72-108). I only have higher readings in the morning. Any official fasting blood tests have been performed in the morning after swimming. Should I take my next fasting blood test a couple of hours later? Would appreciate any suggestions on reducing my waking blood sugar.
Hanah, it’s great that you’re so active! What you’re seeing in this situation is likely due to the body’s natural glucose response to exercise. When you swim, your body releases stored glucose from the liver to fuel your muscles, which can cause a temporary rise in blood sugar—this is completely normal. Alongside exercise it can be common for people to see a temporary rise in blood glucose levels. Since official fasting blood tests are typically done after 8–12 hours of fasting, it’s best to take them before exercise rather than after, as post-exercise readings don’t reflect true fasting levels. So you say your reading upon waking is 6.2 or 111, that’s your fasting number and it’s within an acceptable range and not far from the normal range, so making some minor adjustments may help fine-tune your morning readings. We had some suggestions on doing that in episode 38. Your numbers are in a good range most of the day, so that’s fantastic to hear and keep up the great work! If you have an ‘official’ fasting test via the pathology lab, definitely consider doing this before exercise for a better reflection of that fasting number.
10:16
Susan said: I am concerned about my fasting blood sugar levels. Upon rising, I measure my blood sugar. Some days it is normal and other days it isn’t. For example, my blood sugar was 113. An hour later, it had risen to 155 even though I had not eaten or drank anything. This has been occurring periodically for the last two months. Please help me understand what is happening to my body.
Susan, as we’ve mentioned a few times already, what you’re describing is likely due to the dawn phenomenon. In the early morning, your body releases hormones (like cortisol and glucagon) to prepare for the day, prompting your liver to release stored glucose, which can raise blood sugar. We discussed why and how this happens, in detail in episode 38.
It could also be due to the feet-on-the-floor effect. Simply getting up and moving around can trigger a type of stress response, leading to increased levels of cortisol and adrenaline that spike glucose release from the liver, even without eating. For many people affected by this, it helps to eat something – a small handful of nuts for example and some people keep their nuts beside the bed. And it often helps to eat breakfast before trying to do too many things, even something as mundane as doing a bit of housework, preferably eating a low carb breakfast with lots of fat and protein. You can also try implementing some strategies we spoke about in episode 38 to help improve morning levels. And if you’re one of our members experiencing similar issues, view the new healthmap on lowering blood sugar for additional steps you can take.
12:26
Francinah said: My morning blood glucose levels are above 8 to 10.5 most of the days. What can be the solution to this?
Francinah, consistently high morning blood sugar (8–10.5 mmol/L or 144–189 mg/dL) suggests that overnight glucose production is a key factor. The main causes could be the dawn phenomenon (early morning hormone-driven glucose release) or prolonged elevated blood sugar from the previous day’s meals. In episode 38 we talked about why morning blood sugar is often high, so we’re not going to go into detail here but it is often related to hormonal changes early in the morning, that dawn phenomenon. You can still have some influence over this by making adjustments to your nutrition and lifestyle. The first thing to consider though is whether your A1c is high or your post-meal glucose readings. If your A1c is high, it’s unlikely that your morning blood sugar will lower, so your first step is to address the A1c level, aiming for 7% or even better, under 6% and you can do this primarily by adjusting your nutrition plan. Once your A1c numbers are in a healthy range, it can still take a while for morning numbers to balance, up to two years in some cases. But if your A1c and post-meal numbers look good, then give it some time and apply some other strategies that we talked about in episode 38 – assessing your nutrition, cheese and apple cider before bed, natural supplements, meal timing, assessing sleep and stress – there are a lot of factors you can look toward and there are lots of science-backed strategies that help to lower those morning numbers.
14:58
Okay, the last question for the day comes from Rebecca who left us a voice message. Let’s listen to that now.
Rebecca’s voicemail: “Hello, this is Rebecca Wilson. They sent me the email regarding the fasting in the morning. I’m type 2 diabetic, a year and a half now, and I worked really hard for a year and a half to get my A1C from 13 to 7, and now it’s up to 9, but it’s probably getting higher. The last month or so my sugars are staying around 290, 280, to 300, and I’m not sure why. My eating habits are back to just salads, and vegetables, and fruits, and protein, and I’m not exercising as much, but I’m going to start that, but my sugars are about 300 in the morning, 280, and I’m fasting until about 1, because if I eat in an hour, it’s going to get higher, and so I’ve been trying to until about 1, so that when I do eat, you know, it gives it time to come down, and then when I eat, it’s not going to be extremely high, but I’m also losing weight. I’ve lost another 5 pounds.”
This is an interesting scenario and since we don’t have the whole story, we have to try to fill in the gaps here. Rebecca has an A1c that seems to be increasing quite rapidly, despite her eating habits being relatively healthy, sugars that are staying high even though it sounds like those meals are low in carbohydrates, fear of eating in the morning so as not to increase blood glucose spikes even higher, and weight loss, which sounds unintentional the way Rebecca suggests it.
Even though you’re not doing as much exercise it sounds like you’re doing some. And even though it sounds like you’ve pulled your diet right back into alignment, it sounds like these elevations have occurred despite a relatively healthy routine. The persistently high blood sugar, even while fasting, suggests inadequate insulin action so we’d be thinking insulin resistance, which is common in type 2 diabetes, but in this case it sounds more like insulin deficiency worsening. This could indicate progression of beta-cell dysfunction, common in type 2 diabetes over time and unusual in those newly diagnosed. While the weight loss could be due to the fasting and dietary intake, losing weight while having high blood sugar raises concerns about unintentional weight loss, which again could potentially point toward significant insulin deficiency, or in other words, your body may not be producing enough insulin.
The first thing to question is whether you have Latent Autoimmune Diabetes in Adults, called LADA for short, which is often misdiagnosed as type 2 diabetes. LADA is an autoimmune form of diabetes like type 1, but with a slower onset. LADA is also known as Type 1.5 Diabetes, as it has characteristics of type 1 and type 2 diabetes and it’s often misdiagnosed as type 2 diabetes. The pattern that you’re suggesting sounds like a common scenario seen in LADA. Being that you were diagnosed not long ago, we don’t know if you’re taking medications but you had a good initial response to your diet and lifestyle strategy with your A1c going from 13 to 7, but now you’re seeing sharp rises across all your blood sugar metrics and you’re experiencing weight loss. These can all be classic signs of LADA. So one of the first things to do to rule this out is to get some tests from your doctor to test antibodies and c-peptide. Since in LADA there is some beta-cell dysfunction in the pancreas and there can be a gradual deficiency in circulating insulin, treatment is different from type 2 diabetes and most people need small doses of insulin. This is important because you don’t want to delay proper treatment and risk developing complications.
Of course, it may be attributable to other factors – maybe the prolonged fasting is backfiring contributing to higher fasting glucose so perhaps you could try a small protein- or fat-based snack or meal first thing in the morning to evaluate what happens. A small, early meal may help suppress excess liver glucose production and stabilize blood sugars later in the day. We don’t know what your eating habits or nutrition plan have been like, so you could look at exploring adjustments here. You could look toward reintroducing movement as we know exercise can help lower glucose. Adjusting carbohydrate intake, eating earlier in the day, and reintroducing movement might help stabilize blood glucose levels. It would also be important to evaluate whether there has been anything else in the past couple of months that may have contributed to this rise in blood sugar – illness, infection or stress for example. Troubleshooting all these things may be useful, but the first step would be having some tests to ensure your diagnosis is accurate, so you can assess the next best steps to take given the circumstances. If you do have LADA, then your course of treatment will be different. If you don’t, then various other factors need to be assessed more closely. If you need help to do that, the best course of action for you is personal one-on-one nutrition coaching with someone like myself, as you need that dedicated attention to help troubleshoot more complex issues like this. You can find out more about getting personal help on our website.
Well, that’s all for today’s episode!
We’ve covered why fasting blood sugar levels fluctuate, what’s considered normal, some of the best ways to lower those morning numbers naturally, which you can also learn more about in episode 38, and we’ve covered some troubleshooting tactics for more complex situations where things don’t seem right with blood sugar numbers, despite your best efforts. I hope you’ve found some useful tips and insights you can apply to your own situation to get better results.
Remember, if you’re one of our members, we have our new healthmap for lowering morning blood sugar levels now available for you, providing a clear, step-by-step process to lower those fasting levels naturally, with detailed information and checklists to guide the process.
Thanks for tuning in, and I’ll see you next time!
Dr Jedha, over and out.
NOT PART OF TRANSCRIPT
Rebecca, Type 2 Diabetes 1.5 years, got A1c from 13 to 7 but now it’s up to 9 and it’s probably getting higher the last month or so, my sugars are staying around 280-300 and I’m not sure why. My eating habits are back to salads, vegetables, fruits, protein, not as much exercise. Sugars in the morning are about 300. Fasting until about 1pm cos if I eat, it’s going to get higher, so I’ve been fasting until 1 to give it time to come down and then when I eat it’s not going to be extremely high. But I’m also losing weight, I’ve lost another 5 pounds so any advice is appreciated.
AManda said: l am someone who suffers from bad health anxiety and whenever l am coming up to blood work l get myself worked up 😢 My last blood test recently had my fbg at 7 but my Hba1c at 5.6. My GP still said l now have type 2 and lm not sure what to believe as l know stress can affect fbg levels but she just brushed me off when l said but my Hba1c is more indicative of my actual blood sugars level overall.
REPLY: a fbg of ≥7 is one criteria used for diagnosing diabetes, but if you have no other symptoms, the medical care guidelines outline that you need to have at least two fbg tests ≥7 to determine diabetes. A diagnosis of diabetes should not be given from a single high fbg test, especially given your HbA1c is perfectly normal. Anxiety can certainly influence fbg, so definitely something to take into consideration.
So if my Hba1c was 5.5 that means my overall glucose levels for past 3 mths are good, confusing as my fbg was 7 on the one occasion it was tested, Was feeling stressed though at time of blood being drawn, seem to do this to myself prior to any sort of test ( like white coat syndrome ) 😪
REPLY: Yes, a Hba1c of 5.5 suggests your daily levels are good. FBG can be different, influenced by wake-me-up hormones.
Thanks for that.So why do doctors use FBG to diagnose diabetes as many things can influence the reading. Also can the dawn phenomenon affect reading if you have blood drawn for test ar say 10 am and you are not yet diagnosed as diabetic ?
REPLY: Many things won’t influence the reading unless there is the presence of diabetes, as the dawn phenomenon usually only impacts those with insulin resistance/diabetes.
Grab Your Free Copy To Lower Fasting Blood Sugar Levels
A mini e-guide with Scientifically Proven Strategies that actually work!
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…



Leave a Reply