While there are more effective treatments, like diet and lifestyle, the default treatment method for type 2 diabetes is to prescribe medications.
But what you need to understand is that just because prescribing medications is common, it doesn’t necessarily make it good practice. All medications come with a downside—side effects, including medications that lower blood sugar.
In fact, diabetes medications in people 65+ years are among the most common drug types for hospital emergency visits—their therapeutic use can and does cause harm; with over 38% of people who end up in hospital requiring subsequent hospital visits.
If your doctor wants to prescribe medication, you need to be informed of each medication and its side effects, because it is largely up to you to take charge of your health. So let’s look closer at the mechanisms and side effects of various type 2 diabetes medications.
Overview of Type 2 Diabetes Medications
It’s not uncommon for people with type 2 diabetes to be prescribed one or more medications with the goal of lowering A1c levels. Each medication has distinct mechanisms of action and side effects.
Commonly prescribed classes include Metformin, Sulfonylureas, DPP-4 inhibitors, SGLT-2 Inhibitors, and GLP-1 Agonists; and insulin can be prescribed in some cases.
NOTE: Always consult with your doctor before making changes to your medications.
Diabetes Medication Mechanisms
1. Metformin (biguanide): Metformin is the most commonly prescribed oral medication for both type 2 diabetes and prediabetes. Metformin works by reducing the liver’s glucose production and boosting cell sensitivity to insulin. The maximum effect at the highest dosage is a 1.5% A1c reduction.
2. Sulfonylureas: These oral agents, such as Glipizide (Glucotrol), Glyburide (Micronase, Glynase, Diabeta), and Glimepiride (Amaryl), stimulate the pancreas to produce more insulin. The maximum effect at the highest dosage is a 1.5% A1c reduction.
3. DPP-4 inhibitors: These oral medications, Sitagliptin (Januvia), Saxagliptin (Onglyza), Linagliptin (Tradjenta), and Alogliptin (Nesina), enhance the action of incretin hormones, leading to increased insulin secretion. The maximum effect at the highest dosage is a 0.7% A1c reduction.
4. SGLT-2 Inhibitors: Oral drugs like Canagliflozin (Invokana), Dapagliflozin (Farxiga), Empagliflozin (Jardiance), take an unusual route—they facilitate glucose excretion through the urine by inhibiting renal glucose reabsorption. The maximum effect at the highest dosage is a 0.7% A1c reduction.
5. GLP-1 Agonists: These are injectable medications. The most commonly prescribed are Dulaglutide (Trulicity), and semaglutide (Ozempic/Wegovy). These increase insulin secretion and suppress glucagon release in a glucose-dependent manner. The maximum effect at the highest dosage is a 1.4% A1c reduction.
6. Insulin: Insulin is an injectable medication. In type 2 diabetes, insulin is not prescribed as frequently as other medications, as it is only necessary where the pancreas is no longer producing sufficient insulin. Unlike other diabetes medications that stimulate the body to produce more insulin or improve its effectiveness, insulin therapy (from rapid-acting to ultra long-acting insulin) involves the direct administration of insulin to the body to regulate blood sugar levels. The maximum effect of insulin per 1 unit/kg is 2.5%.
Of course, this isn’t a list of every medication because there are others, along with combo meds as well.
Let’s just put something into perspective. If your A1c is 10% and you need to get it down to 7%, you would likely be prescribed multiple medications (excluding insulin) to do that.
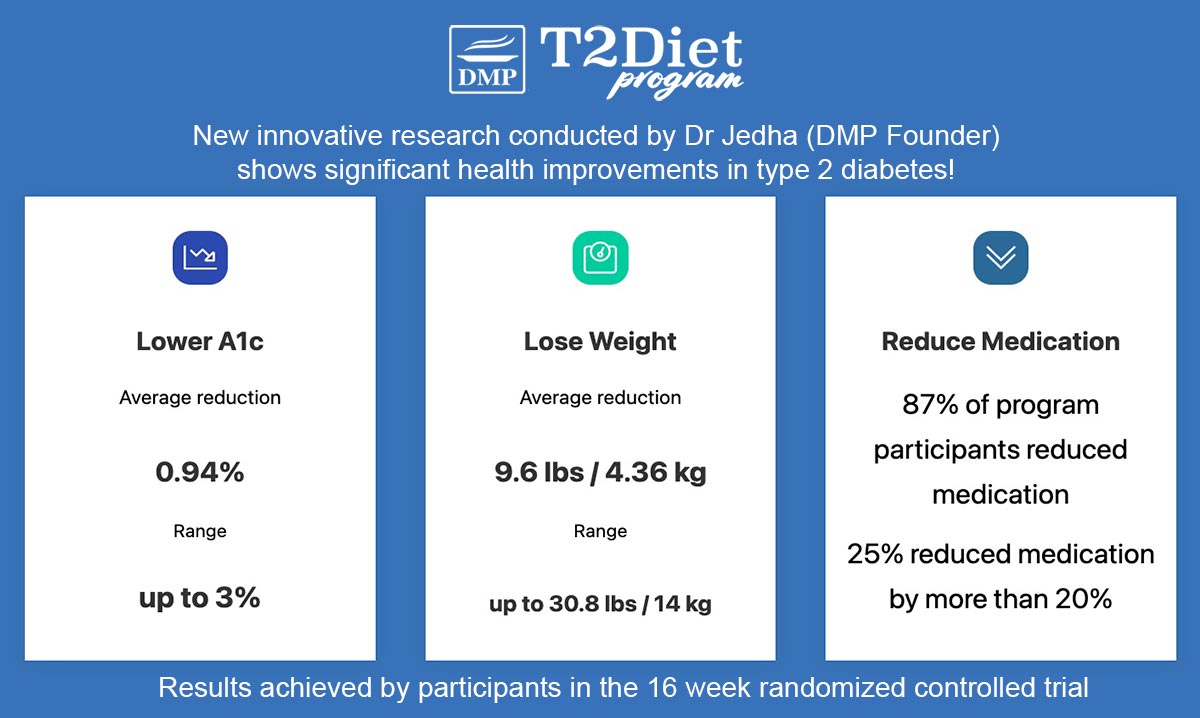
But, you can lower A1c by 3% in 16 weeks through diet and nutrition, so you really have to question the overall benefits, especially given all medications come with potential side effects.
When I started the program my HbA1c was 9 or 10%. At the end of the program it was down to 6%, which was amazing! And I was able to reduce medication, and it just worked really well. It’s now been over a year and I’ve been able to prove it’s sustainable. I was just blown away by the result. ~John
Side Effects of Glucose-Lowering Medications
Across all diabetes medications, blurred vision and weakness are two of the most common side effects, along with lightheadedness.
These are symptoms may seem harmless and they can easily be overlooked, but what if they result in a fall and bone fracture? That’s not harmless, so please don’t discount anything you feel as a potential side effect of your medications.
Each medication class comes with its potential side effects:
1. Metformin: The most common side effect people experience from Metformin is gastrointestinal disturbances such as nausea and diarrhea. Starting at a very low dose and gradually increasing the dose in increments can help minimize discomfort.
Long-term use of Metformin may also lead to vitamin B12 deficiency. The longer you take it, the greater this risk, especially if taking 4.5 years or longer, so be sure to have your vitamin B12 checked periodically.
2. Sulfonylureas: The biggest concern with these is they cause hypoglycemia (low blood sugar) and because they increase insulin, they also cause weight gain. Some people may experience skin reactions. They may be linked with ischemic preconditioning, which may lead to heart disease or cardiac events over time. And, these medications do become less effective over time.
3. DPP-4 inhibitors: Generally these medications are well-tolerated, but potential side effects include joint pain, fluid retention and risk of pancreatitis.
4. SGLT-2 Inhibitors: These medications are associated with increased risk of urinary tract infections and genital mycotic infections. Because they alter fluid volume and lower blood pressure they can cause dizziness. They have been linked with elevation in LDL cholesterol levels. There have been some rare cases of diabetic ketoacidosis, usually linked to a major event such as surgery, extreme stress or illness, which is why doctors frequently take you off these medications prior to any major life events.
5. GLP-1 Agonists: These medications, particularly semaglutide’s (Ozempic/Wegovy) have taken the world by storm the past few years, flooding the market. But, it is important to recognize the concern over side effects, which have been increasing with the more people who use them.
Gastrointestinal side effects are very common—people find it difficult to hold down food/ hold in food, so things like nausea, vomiting and diarrhea are common and can be severe, leading to hospitalization in some people. There is also a risk of pancreatitis and thyroid tumors.
Another serious side effect is ileus, which refers to intestinal blockage. This was added as a side effect to the drug labeling for Ozempic in September 2023 and is true for Wegovy as well. Symptoms such as cramping, pain and inability to have a bowel movement should be monitored closely. The condition can be fatal if not treated.
6. Insulin: The most common side effect associated with insulin therapy is hypoglycemia, or low blood sugar, which can occur if insulin doses are too high relative to the body’s needs. Symptoms of hypoglycemia include dizziness, sweating, confusion, and, in severe cases, loss of consciousness.
Weight gain is another side effect, as insulin can increase fat storage in the body. Additionally, some people may experience injection site reactions, including redness, swelling, and pain. Long-term use of insulin can also lead to worsening insulin resistance, necessitating adjustments in dosage or insulin type.
NOTE: Always consult with your doctor before making changes to your medications.
Type 2 Diabetes Medication Alternatives
While prescribing medications may be common, many people don’t realize they don’t necessarily need to take medications, that there is another way, a natural way that can get incredible results.
What is this way to reduce or stop medications? It’s diet and nutrition!
Diet and nutrition is the #1 treatment strategy for type 2 diabetes – often being more effective than medication. We know because we’ve been helping people with type 2 diabetes and prediabetes treat their condition naturally, for the past decade – supporting them to reduce and stop medications, with incredible results!
We’ve got hundreds of testimonials but here’s what a couple of people have said:
My weight dropped 6 pounds (2.7kg), and my A1C dropped to 5.8! This was an all-time low for me. Best of all, my doctor reduced my daily amounts of metformin and glipizide by half: The same tablets one time daily! Fast forward 4 years: I continue to do well! At 70 years old, my HbA1C continues to be under control. My cholesterol continues to be controlled. I maintain lower medication. ~Sheryl
When I started DMP, I was 310 lbs (140kg) and my A1C was 10. I had a very unhealthy lifestyle. Since then, I have lost weight, I am at 190 lbs (86kg) now and my A1C is between 6.5 to 7.0 and no longer have to take medicine. Thank you for what you do!” ~Dusty
Here at DMP, we’ve also conducted scientific research and proven our natural nutrition approach works – with 87% of people reducing medication in just 16 weeks, by taking the T2Diet Program!
Inside our exclusive members site, we also have hundreds of resources to support our members to implement natural diabetes treatment strategies, and how to use effective natural therapeutic supplements, and much more.
Conclusion: Type 2 Diabetes Medications
The range of medications available for type 2 diabetes treatment offers multiple pathways to help you manage your condition effectively. However, it is crucial to be aware of the specific actions and potential side effects of these medications, some of which can be serious.
Importantly, if you do take glucose-lowering medication, you need to have your medication reviewed frequently, because in many cases, you do not need to keep taking medications forever. Every 3-6 months is what the medical care guidelines recommend, but we know many doctors are not doing that, so it is up to you to take charge of your health.
It is also important to be aware that when it comes to lowering blood sugar and A1c, natural treatment options such as the right diet and nutrition plan can be as effective, if not more effective than medications.
We’ve proven this in our T2Diet Program, where 87% of people reduced medication in just 16 weeks, and some people reduced their A1c by 3% in 16 weeks – that’s much more powerful than medications!
KNOW THIS: If you take a proactive approach, you can not only avoid medications, but you can work with your doctor to reduce and get off medications too!
Join Us As A Member Today – let us support you to reduce or stop your meds – we’ve helped many, many people before you and it certainly makes a BIG difference to your life!



darlene
Can Metformin cause kidney failure?
Dr Jedha
Hi Darlene, Metformin itself doesn’t cause kidney failure, but it’s not recommended for people with significantly impaired kidney function.
darlene
What does it to the kidneys so that it would not be recommended?
darlene
By the way I forgot to thank you for answering my question. Thank you so much!!!!
RockT
This article mentions reducing A1C from 10% to 7%. It also mentions metformin can reduce A1c by up to 1.5% at maximum dosage. I didn’t think A1c was a percentage of measurement. Please explain.
Dr Jedha
Hey RockT, yes, A1c is most commonly measured in percentage and in research studies they always use percentage as well. In some countries, A1c is measured in mmol/mol instead of a percentage so perhaps that’s the case for you. Here’s more info on A1c and the translation between the two measurements.
Dharam Lingham
Yes it’s good one