Table of Contents[Hide][Show]
- LISTEN TO THE PODCAST
- CHAPTERS
- Unveiling Insulin’s Role
- What is Insulin Resistance?
- The Ripple Effect of Insulin Resistance
- 4 Things That Drive Up Insulin
- Development of Insulin Resistance
- Dietary Culprits of Insulin Resistance
- Diabetes is Insulin Resistance of the Liver
- Interventions for Insulin Resistance: Diet and Beyond
- Transcript
Insulin is a key hormone involved in blood sugar regulation. But in diabetes, insulin struggles to work effectively – a condition called insulin resistance. Insulin resistance at the level of the liver, is essentially the underlying cause of prediabetes and type 2 diabetes. And with insulin resistance, there are a range of other metabolic issues that can occur – weight gain, high blood pressure and cholesterol, inflammation and more.
The good news is, you can change it! Primarily through diet and nutrition, insulin resistance can be reversed.
LISTEN TO THE PODCAST
CHAPTERS
2:22 The role of insulin
4:35 Insulin resistance defined
5:40 The liver and insulin resistance
8:21 Effects of insulin resistance throughout the body
14:56 Cause of insulin resistance
17:17 How carbohydrates create saturated fat
22:57 You can change it all!
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
Unveiling Insulin’s Role
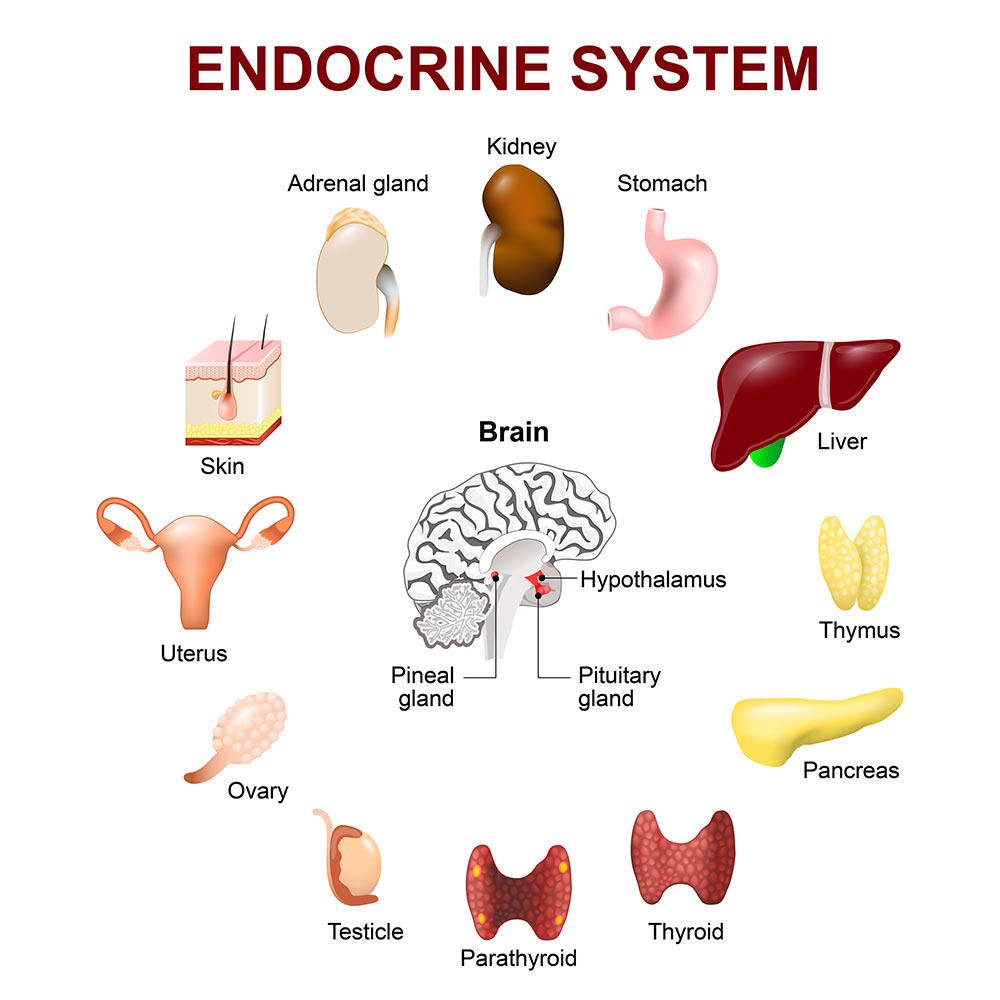
Insulin is a hormone released from the pancreas, one of the body’s endocrine organs.
Insulin action is required throughout the body as the central nervous system uses its signals to control energy metabolism and balance, for reproduction, for brain function, and other functions too.
At its core though, insulin’s primary role is as an energy storage hormone, and its primary role is to facilitate glucose (carbohydrate/sugar) transport into cells.
Beyond its pivotal role in glucose metabolism, insulin’s influence spans across fat storage, protein synthesis, and overall metabolic balance.
What is Insulin Resistance?
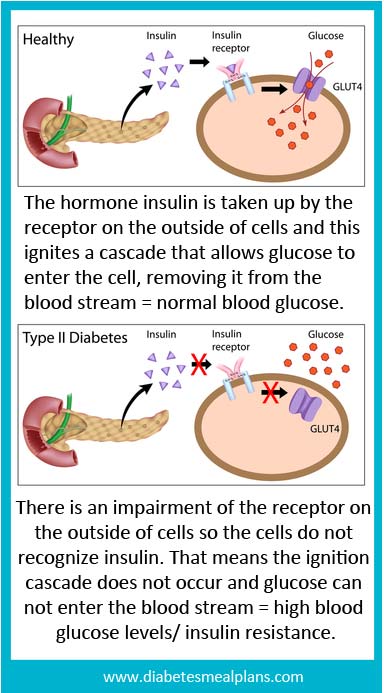
The disruption of insulin’s functionality or its diminished effectiveness is known as insulin resistance.
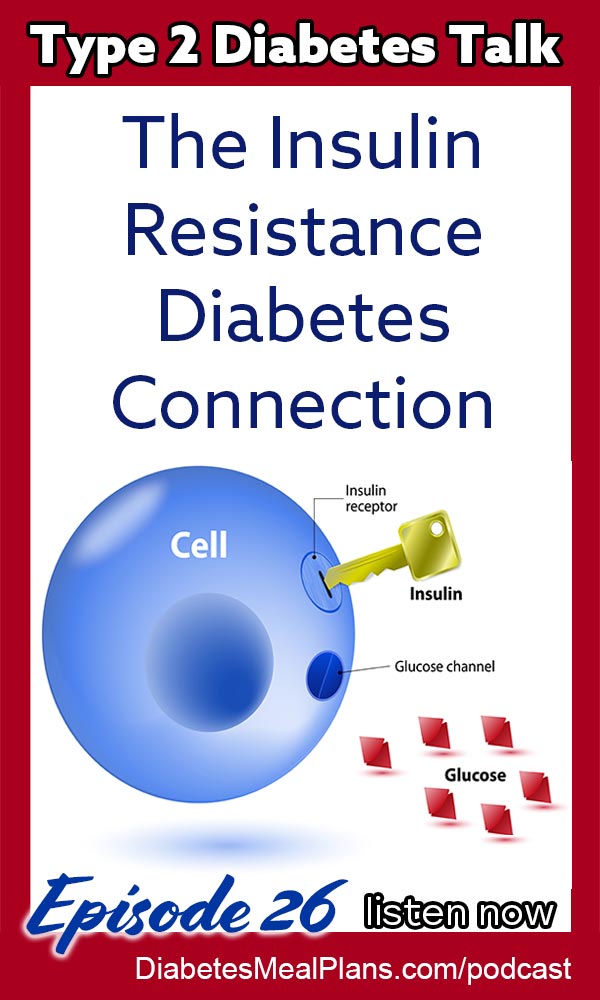
Insulin resistance occurs when the insulin receptor cells do not respond to the action of insulin on those cells – the insulin ‘key’ stops working as it should. The picture below gives a good visual explanation of this process.
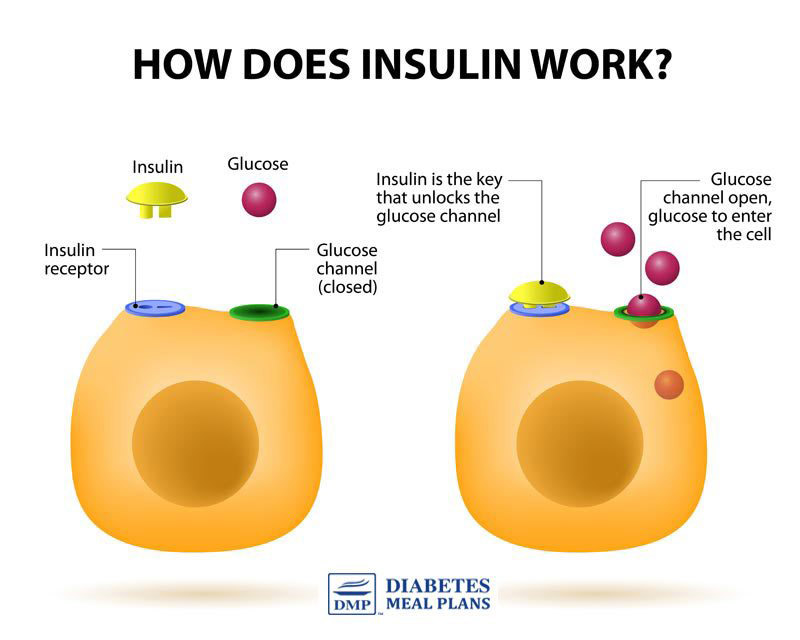
These insulin receptor cells are located in our fat tissue, liver, and muscles and under normal conditions they accept the response of insulin, which helps maintain normal blood glucose levels.
But when the receptors are impaired, glucose can’t enter cells and this results in glucose staying in your bloodstream, meaning high blood glucose.
But, there’s also another problem too – more insulin in your bloodstream.
The Ripple Effect of Insulin Resistance
In insulin resistance, the body’s cells become desensitized to insulin’s glucose-transporting signals, compelling the pancreas to secrete more insulin to maintain glucose balance. Then you have two issues occurring, hyperglycemia (high blood sugar) and hyperinsulinemia (high insulin).
Essentially, we develop a resistance to insulin as a result of sugar and/or insulin overload.
The combined effect of these two issues, not only exacerbates cellular resistance but paves the way for a range of metabolic issues – from non-alcoholic fatty liver, weight gain and cardiovascular disease to hypertension and high cholesterol. In insulin resistance, the web of metabolic dysfunction can become a vicious cycle.
Insulin resistance prevents glucose from entering the cells but it also prevents amino acids from entering cells and we need those for building the body.
As a result of insulin resistance many things can occur in the body including:
- You can lose muscle
- Your energy levels may drop
- Hunger usually increases
- You probably crave more sugar
- You have increased inflammation
- It speeds up aging
- The liver can start to dysfunction
- The body can’t convert thyroid hormones
- You may develop thyroid problems
- Metabolism may slow down
- The whole body can start deteriorating
So as you can see there are many potential negative effects that ripple throughout the body from insulin resistance.
4 Things That Drive Up Insulin
Keeping blood sugar levels in a healthy range is important, but being mindful of contributors of insulin spikes is also important for our health and decreasing insulin resistance.
Here’s 4 things that can drive up insulin:
1. Insulin rises in response to a meal, especially one filled with refined sugar and carbohydrates, or too many carbohydrates at one time.
2. Because of specific foods you eat…you can develop a fatty liver and develop insulin resistance, then your pancreas has to produce more insulin to force the liver to do its job plus deal with blood sugar.
3. Increased cortisol – your stress hormone – increases the likelihood of developing insulin resistance, increases blood glucose and increases production of insulin.
4. Three classes of pharmaceutical drugs that drive insulin up – steroids to control inflammation, anti-psychotics to stabilize mood, and some oral medicines for diabetes.
Development of Insulin Resistance
Due to the complexities of the body, the debate about the exact cause behind insulin resistance continues – the exact mechanisms are still largely unknown.
Scientific evidence however, pinpoints diet-induced inflammation as a prime suspect in the onset of insulin resistance. The inflammatory process, particularly at the cellular level, interrupts insulin signaling pathways, leading to decreased insulin efficacy.
Notably, research suggests that insulin resistance can initiate within the brain, specifically the hypothalamus (a key endocrine organ – see image above). Within the hypothalamus, inflammation disrupts the satiety signaling of insulin and leptin, another hormone critical for appetite regulation, along with ghrelin, the hunger hormone.
According to research, inflammation in the hypothalamus is largely diet-induced. Or in other words, what we eat is driving inflammation and insulin resistance.
Dietary Culprits of Insulin Resistance
The dietary influence on insulin resistance is multifaceted, with high sugar and carbohydrate consumption playing leading roles.
High amounts of carbohydrate prompt sharp insulin responses, contributing to the overload that eventually desensitizes cellular receptors. Excess carbohydrate intake also leads the liver to produce a saturated fat called palmitic acid.
Out there on the wild west web you may hear people say saturated fat causes insulin resistance, but they fail to tell you that it’s excess carbohydrate that prompts the liver to produce saturated fat internally – in the form of palmitic acid.
Sugar and carbs are the problem, not saturated fat!
That said, the type of fats in our diet are very important. Limiting intake of low quality inflammatory oils like vegetable oils, peanut, soy, and safflower oils is key, as these oils increase inflammation in the body’s cells as well.
In addition, limiting intake of processed and packaged foods that are not natural nutrient dense foods to support the body, is highly recommended.
Diabetes is Insulin Resistance of the Liver
The liver, a central hub in glucose metabolism, plays a pivotal role in maintaining blood sugar levels within a tightly controlled range. It regulates glucose storage and release through intricate mechanisms, guided largely by insulin.
Under normal circumstances, insulin signals the liver to convert excess glucose from the blood into glycogen for storage, effectively lowering blood sugar levels post-meal. Conversely, in periods of fasting or low blood sugar, insulin levels drop, prompting the liver to convert stored glycogen back into glucose, releasing it into the bloodstream to ensure energy supply to the body.
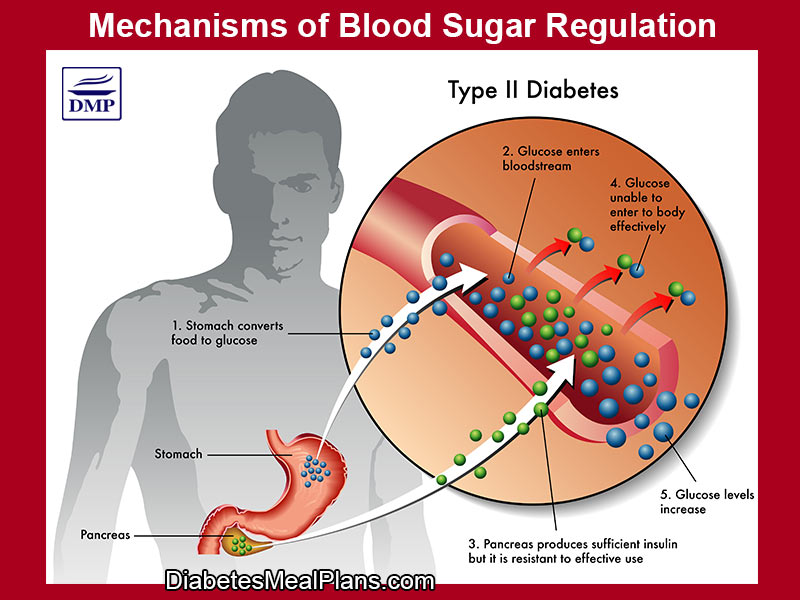
However, in the context of insulin resistance, this finely tuned system falters. The liver’s responsiveness to insulin diminishes, impairing its ability to store glucose as glycogen.
Despite elevated levels of insulin, the liver fails to halt glucose production and release effectively. This paradoxical increase in liver glucose production, despite the presence of high insulin levels, underscores the liver’s pivotal role in the development and progression of type 2 diabetes.
Insulin resistance in the liver not only disrupts glucose metabolism but also affects lipid metabolism. It contributes to increased production of triglycerides, leading to a cascade of metabolic disturbances including abnormal cholesterol levels—an increase in triglycerides, a decrease in HDL cholesterol (“the good cholesterol”), and a rise in small, dense LDL particles, which contribute significantly to cardiovascular disease risk.
Interventions for Insulin Resistance: Diet and Beyond
The good news is that the body is very intelligent, so if you start today, you have an opportunity to turn it all around. The solution however is not medication.
Reversing insulin resistance needs a comprehensive natural approach, emphasizing diet and nutrition – that is going to be your primary treatment strategy. A low-carbohydrate diet, rich in whole foods, ample fiber and healthy fats is key.
Other aspects of your health to consider are physical activity and stress management. Regular exercise enhances insulin sensitivity, further supporting glucose regulation. Reductions in stress helps to reduce cortisol (which stimulates blood sugar and insulin) and balance hormones.
In addition, therapeutic supplements like berberine, known for its glucose-lowering effects, provide a complementary strategy to improve insulin sensitivity.
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful people and welcome to episode 26 where we’re going to delve a little deeper into the underlying cause of pre and type 2 diabetes, and the relationship this may have to your other health problems as well.
Next week I’ll be joined by a special guest, a medical doctor and we’ll be chatting about humanized medicine to reduce medications. Interested to find out what humanized medicine is? Well, I guess you’ll have to tune in for this very interesting discussion.
Getting back on track for today…back in episode 12 we talked about weight loss and we explored the Carbohydrate Insulin Model, and how this model helps us understand the physiological reasons of why we might gain weight and how we can lose it too. We explored one particular hormone, insulin, and today we’re diving a bit deeper to explore the impact of insulin on the body and how changes in the function of this hormone at a cellular level, not only influences our weight, but leads to the development of pre and type 2 diabetes, and has many influences on other aspects of our health as well.
1:20
To begin, let’s look at this whole blood sugar regulation thing.
Whether we have diabetes or not, our body has a certain level of blood sugar balance that it tries to keep within a fine margin and the body does this to keep us safe, because if we have too much sugar in the blood it causes damage to the lining of our arteries and small vessels throughout the body. The body is really quite incredible when it comes to balancing systems, which occurs through a complex array of hormonal responses that occur.
Insulin is a hormone in our body made by an organ called the pancreas. Insulin is crucial for maintaining energy balance and ensuring that cells have access to the nutrients they need for proper functioning. Insulin action is required throughout the body as the central nervous system uses its signals to control energy metabolism and balance, for reproduction, for brain function, and other functions too. Insulin has roles in glucose uptake, glycogen synthesis, fat storage, protein synthesis and overall metabolic health. But, one of the main roles of insulin is as an energy storage hormone, to help push energy, primarily from carbohydrate, out of the blood and into the body’s tissues. Insulin is the primary hormone that helps the body control the levels of sugar in the blood.
When we eat a meal, insulin is released from the pancreas to help our body regulate the energy and keep our blood sugar levels balanced. One major issue we face with our modern diets is we keep feeding our bodies high levels of sugar and carbohydrates, along with processed foods and low quality inflammatory oils. Then the sugar levels in the blood stay high and the pancreas keeps doing its job to try to regulate that, overproducing insulin to try to compensate for the problem.
4:35
Then we have two issues occurring, both high blood sugar and high insulin and both of these things promote insulin resistance. The cells in our body have receptors that respond to insulin. Normally, when insulin comes in, it acts as a key to unlock the cells so that excess glucose from the bloodstream can flow into the cells. But with high glucose and high insulin the key stops working efficiently, it’s not unlocking the cells because the cells are either less responsive or because there is an overflow of sugar in the body or blood already – there’s two schools of thought here, but either way, we know that the presence of high glucose and high insulin leads to insulin resistance.
To put it more simply, insulin resistance is defined as: a condition in which cells are no longer responding appropriately to circulating insulin.
5:40
Let’s look a little closer at the role of insulin in the liver and the effects of insulin resistance, because in diabetes insulin resistance occurs at the level of the liver.
In the liver, insulin helps regulate glucose storage and release. Insulin signals the liver to take up glucose from the bloodstream and store it as glycogen, a storage form of glucose. When blood glucose levels are low, insulin levels drop, prompting the liver to convert glycogen back into glucose and release it into the bloodstream. In insulin resistance, the liver’s response to insulin decreases and glucose storage is impaired.
Under normal circumstances, insulin helps inhibit a process called gluconeogenesis. Gluconeogenesis is the process where the liver produces glucose from non-carbohydrate sources, like protein for example. After a meal when insulin levels are high, the body would normally suppress gluconeogenesis, helping blood sugar levels to come back into balance. With insulin resistance, even though there are high levels of insulin, gluconeogenesis is not inhibited like normal, but instead it increases so that the liver is also producing and releasing glucose into the bloodstream, which can make blood sugar levels higher.
Insulin also plays a role in fat metabolism and the synthesis of fatty acids in the liver. Insulin resistance can lead to increased production of fatty acids and contribute to abnormal cholesterol levels that increase cardiovascular disease risk.
Insulin resistance also promotes an increased accumulation of fat in the liver (non-alcoholic fatty liver disease or fatty liver), which can lead to liver inflammation and damage. In fact, one of the main drivers of insulin resistance is liver fat.
Insulin resistance has a major impact on our metabolism, triggering a cascade effect throughout the body.
For example, due to the insulin resistance, the liver continues to produce glucose despite elevated insulin levels, blood glucose levels rise, leading to hyperglycemia (high blood sugar) – hence the development of pre and T2Diabetes.
8:21
As we’ve already spoken about, the pancreas initially responds by producing more insulin so in most cases people’s pancreas is fine, but then you have hyperinsulinemia. This hyperinsulinemia further exacerbates insulin resistance in a repetitive cycle. Over time the pancreas also deposits fat, so eventually this affects the production of insulin itself, so as people develop along the diabetes spectrum and if it’s not addressed this can lead to decreased insulin production.
Insulin resistance contributes to high cholesterol and altered cholesterol profiles, frequently increasing triglycerides, decreasing HDL cholesterol the “good” cholesterol, and increasing the type of LDL particles that contribute to heart disease – small dense LDL particles.
Insulin resistance promotes chronic low grade inflammation throughout the body’s cells and increases oxidative stress, which can damage our cells and tissues. This inflammation can aggravate insulin resistance and diabetes.
Insulin resistance causes sodium retention in the kidneys, contributing to high blood pressure levels. Insulin resistance is also associated with increased sympathetic nervous system activity, which can further contribute to high blood pressure by increasing heart rate and constricting blood vessels.
Insulin resistance can contribute to weight gain, as we discussed in episode 12, and weight gain further aggravates insulin resistance and promotes inflammation. High insulin and insulin resistance also stops us from losing weight by inhibiting the breakdown of stored fat.
Insulin resistance also impacts other hormones involved in appetite control such as leptin and ghrelin and that can further complicate metabolism and weight control.
As a result of insulin resistance many things can occur in the body including:
- You can lose muscle
- Your energy levels may drop
- Hunger usually increases
- You probably crave more sugar
- It speeds up aging
- The body struggles to convert thyroid hormones
- You may develop thyroid problems
Prediabetes and type 2 diabetes are insulin resistance at the level of the liver. Research shows us that heart disease is insulin resistance at the level of the cardiovascular system. And there is now research showing insulin resistance in the brain linked to dementia and Alzeimer’s. Insulin resistance can influence so many things. As you can see, the cascade effect that occurs from one thing to another can have profound effects on your body and your health overall. But the positive part of all this is that your body is very smart. It’s doing all this to protect you, because our body is designed to have blood sugar levels within a certain range. If our body just lets sugar go to all sorts of unwieldy levels, the sustained high blood sugar can damage blood vessels and nerves over time, and this is what leads to complications such as neuropathy, retinopathy, and other conditions.
Our body doesn’t want that, so it is doing all these things to protect us from getting sick. It is doing its job to try to balance everything the best it can, and often, we’re not doing a very good job to support it. We might be eating way too much sugar, refined carbohydrates and junk food. We might be doing no exercise at all. We might be experiencing high and prolonged levels of stress. We might lack sleep. We might be exposed to any number of environmental toxins. In today’s modern world, we have a lot of exposures that can influence our health and contribute to the body’s imbalances. But, the positive part of all this is that your body is very smart, so when we can look at our lives and turn some of these things around, our body can come back into balance.
For example, we can choose to eat in a way that supports optimal blood sugar levels. We can choose to include regular exercise into our lives. We can try to minimize stress or learn stress management strategies. We can try to improve our sleep quality. We have tools at our disposal to support our body to reverse the cycle. And one of the best tools we have is our diet and nutrition, which we have direct control over most of the time.
As a consequence of eating good quality food and focusing on good quality nutrition, glucose levels come down, insulin levels come down, liver fat goes down, liver function improves, pancreatic fat decreases, insulin function improves, insulin resistance decreases, cholesterol levels normalize, weight comes down, blood pressure improves, inflammation decreases, and your overall metabolism improves.
14:56
So what causes this insulin resistance?
Well, that is still a topic of debate. There have been countless studies trying to establish the exact mechanisms for why insulin resistance occurs, and still it isn’t fully understood. What we do know is there are abnormalities in the insulin signaling pathway, and a lot of the evidence suggests it all begins with diet-induced inflammation.
Some people proclaim it is all the carbs, some proclaim it’s because of too much saturated fat – we’re going to dive into unraveling this a bit more in a moment.
What we do know is that insulin resistance is due to inflammation. Yes, we know inflammation occurs if we kick our toe and it gets red. But what we’re talking about here is inflammatory processes that occur in our body at a cellular level and increased cellular inflammation interrupts insulin’s actions.
Quite fascinatingly, science shows us that insulin resistance starts in the brain, in our central control organ called the hypothalamus. We have nutrient sensors and fatty-acid sensors that can identify the presence of excess calories and saturated fat, one saturated fat in particular, palmitic acid; and where levels of these are high, this causes inflammation in the hypothalamus that disrupts satiety signaling of both the hormone insulin and another hormone called leptin, which is hormone found in a fat cells linked to appetite regulation. Another fascinating thing is that there is a neural network in the pancreas and digestive tract that coordinate insulin release.
From the hypothalamus, inflammation and insulin resistance causes a cascade effect throughout our entire body and the body’s metabolism. All of those things we just covered – the high blood glucose, high insulin, fatty liver, high cholesterol, weight gain, high blood pressure, and the list goes on. It really is quite fascinating, and it’s all controlled by various hormones in our body.
17:17
As I said before, we have nutrient sensors and fatty-acid sensors in our brain that can identify the presence of excess calories and one particular saturated fat – palmitic acid. And often you’ll hear people harp on and on about how saturated fat causes insulin resistance. This never quite made sense to me, especially since we know that high blood sugar, high insulin and insulin resistance leads to increased production of fatty acids in the liver. People demonize saturated fat, but it is a natural component of many nutrient dense whole foods. So being this never did make sense to me—that consumption of saturated fat causes insulin resistance, I thought, it must be a result of the alterations in fatty acids, that must be why we’re seeing this connection in relation to saturated fat. And it turns out that’s absolutely true.
Remember, evidence over opinion people, so let me share the true and factual evidence on this.
Lots of the studies on insulin resistance have been done in animals and when they do these studies they do use high fat diets that are particularly high in saturated fat – that’s how the researchers of these studies induce the outcome; and of course, if you’re feeding a high saturated fat diet of anywhere from 60-95%, then it may induce a certain outcome.
However, when it comes to the average person’s diet, it is not overly high in saturated fat. People just don’t eat 80% of their diet purely from saturated fat. They are not sitting down to chow on 80% of their calories from lard or tallow, that’s just ridiculous.
So, here is an interesting fact that I don’t hear many people talk about. In fact, I don’t recall ever hearing anyone talk about it before, but when we look at the evidence it’s right there.
Okay, when it comes to fats, what we’re really talking about is fatty acids. There are several types of saturated fatty acids, including lauric acid, myristic acid, palmitic acid, stearic acid and others. And as we just established, the saturated fat that influences the hypothalamus is palmitic acid.
Well, what’s not commonly known is that as a result of excess dietary glucose, the liver produces fatty acids that are rich in palmitic acid. Or in other words, as a result of eating too much sugar and carbohydrate, the liver is producing saturated fat internally, in the form of palmitic acid. And it’s this internal production of palmitic acid that forms a large part of the development of insulin resistance.
When we really look at things logically, the problem is not coming from consuming too much saturated fat. The problem is coming from consuming too much sugar, too much carbohydrate, too many processed foods and low quality fatty acids in the diet. The modern Western diet is high in sugar and refined carbs and high in low quality fats, but those fats are generally not saturated fats, that’s a common misunderstanding. Those fats are more commonly low quality inflammatory fats such as commercially-produced seed oils – soybean oil, peanut oil, safflower oil, and vegetable oil. We’ll delve deeper into this topic in future.
In any case, the effects of different fatty acids in insulin resistance is still not fully understood. There are a wide range of changes in fatty acids in the tissues, in the composition of membranes throughout the body, in fatty acid metabolism, the inflammatory effects, the rates of oxidation of different fatty acids, among other things – it’s all quite complex.
But coming back to the fascinating central control organ, the hypothalamus. Interestingly, the hypothalamus senses increases in the free fatty-acid levels in the blood at the surface of the blood–brain-barrier. If those free fatty acids are palmitic acids, the hormone cortisol is stimulated, which increases insulin resistance. In the presence of increased free fatty acids, we start getting what’s called ectopic fat accumulation.
Instead of staying in fat cells, circulating free fatty acids travel throughout the body and they can be taken up by liver and muscle cells, along with cells in the hypothalamus, pancreas, and gastrointestinal tract. Our body is not designed to store large amounts of fat in these cells, so it only exacerbates the situation, driving all those metabolic alterations we covered earlier – the fatty liver, the weight gain, the elevated blood sugar, blood pressure or cholesterol. This cascade of events that happens in the body, happens on a spectrum, over time.
22:57
The important thing to understand is that while things in our bodies are complex and a complex cascade of events happens in our body as a result of one thing or another, we have the power to change it all, and we can do that through diet and lifestyle.
As I said earlier, we can choose to eat in a way that supports optimal blood sugar levels. We can choose to include regular exercise into our lives. We can try to minimize stress or learn stress management strategies. We can try to improve our sleep quality. We can use therapeutic supplements, such as Berberine, which we covered in episode 21, or other therapeutics. We have tools at our disposal to support our body to reverse the cycle. The most important takeaway here is that one of the best tools we have at our disposal to reverse the cycle, to reverse an altered metabolism is our diet and nutrition, which we have direct control over most of the time.
As a consequence of eating good quality food and focusing on good quality nutrition, glucose levels come down, insulin levels come down, liver fat goes down, liver function improves, pancreatic fat decreases, insulin resistance decreases, insulin function improves, cholesterol levels normalize, weight comes down, blood pressure improves, inflammation decreases, and your overall metabolism improves, your overall metabolism comes back into balance.
Reversing the cycle is exactly what we help people do in our programs and services, so if you need help with getting your health on track, head to our website at Type2DiabetesTalk.com. Taking part in our programs will be the best investment you ever make in yourself because you’ll get proven practical support that leads to real results that are sustainable long term.
As I said earlier, next week I’ll be joined by a special guest, a medical doctor to chat about humanized medicine to reduce medications. Be sure to tune in for this very interesting discussion.
See you next week.
Dr Jedha, over and out.
Get started by grabbing a copy of our recommended food list, as it will help guide you on the types of foods to include and avoid.
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…

laurie wilson
can you do low carb when taking jardiance thanks
Dr Jedha - Nutritionist (PhD)
Hi Laurie, yes you can do low carb when taking jardiance, but you do need to take caution.
Ketoacidosis is a very rare adverse event that can happen with jardiance and other SGLT2 inhibitors, the cause of which is not fully known. However, lowering carbohydrate intake has been noted as a caution, but this caution is more for people following keto diets. DMP guidelines are not a keto diet. With our guidelines people have safely continued jardiance, although many also end up stopping this medication because they lower their A1c levels to the normal range.
It is not fully known if lowering carbohydrates causes ketoacidosis, because cases have usually occurred in relation to metabolically stressful events, such as surgery, extensive exercise, heart attack, stroke, severe infections, prolonged fasting, and other stressful physical and medical conditions.
jack murphy
Great post! Thanks for sharing with us:)
Shikha Pandey
I am prediabetic and my fasting sugar is always high. My insulin level is also high. I am also having hypothyroid which may be result of insulin resistance as you mentioned in your blog. I know all that start with the stress. I try to practice yoga and meditation for mitigation of stress. Thanks, DMP team for this informative blog on insulin resistance.