Table of Contents[Hide][Show]
- What Is Insulin Resistance?
- Why Is Testing for Insulin Resistance Important?
- Blood Tests for Insulin Resistance
- Interpreting Fasting Insulin Test Results
- Risk Factors for Insulin Resistance
- The Importance of Early Detection and Lifestyle Intervention
- The Value of Testing Insulin Resistance in Prediabetes and Type 2 Diabetes
- Conclusion
Did you know insulin resistance is a precursor to prediabetes and type 2 diabetes? Being a precursor means insulin resistance comes before a prediabetes or type 2 diabetes diagnosis.
Despite the critical role of insulin resistance in metabolic health, it often goes undetected for years.
Early detection is essential, as insulin resistance can exist for up to a decade before progressing to prediabetes or type 2 diabetes, offering a critical window for intervention.
Strangely though, doctors do not routinely test for insulin resistance, so let’s chat about insulin resistance in more detail, and exactly how you can request an insulin resistance test so you fully understand your risk.
Even if you’re already living with prediabetes or type 2 diabetes, testing for insulin resistance can provide valuable insights to guide more effective treatment strategies, identify why challenges exist and help you improve long-term health outcomes.
What Is Insulin Resistance?
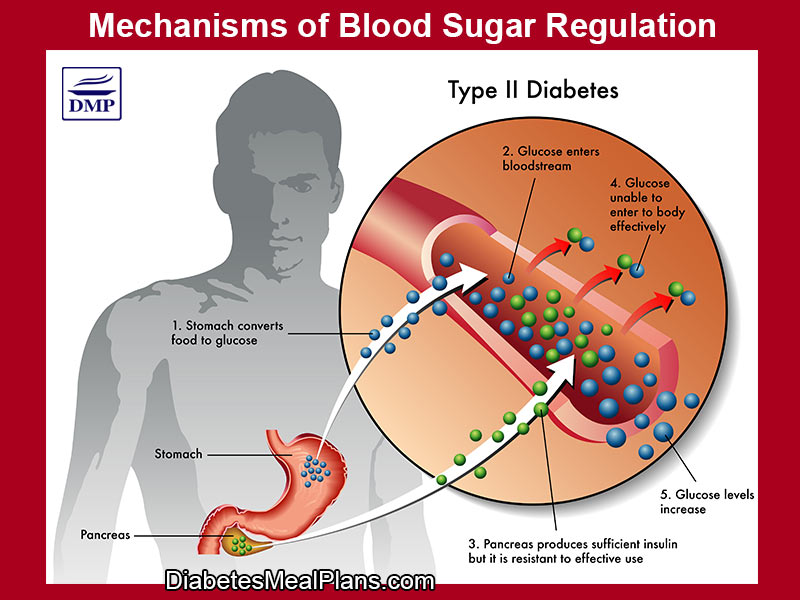
Insulin resistance occurs when the body’s cells become less responsive to insulin, a hormone produced by the pancreas that regulates blood sugar levels.
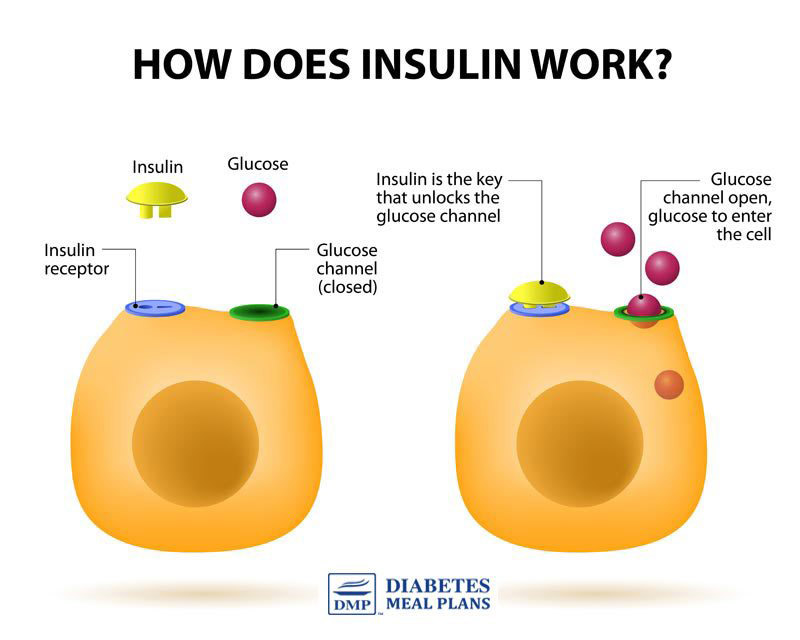
As a result of your cells being less responsive, the pancreas compensates by producing more insulin to maintain normal blood sugar levels.
Over time, this can lead to chronically elevated insulin levels (hyperinsulinemia), and eventually, prediabetes or type 2 diabetes.
Contrary to common belief, insulin resistance and prediabetes are not synonymous.
Prediabetes refers specifically to elevated blood glucose levels that are not yet high enough for a type 2 diabetes diagnosis.
Insulin resistance can exist independently of prediabetes, highlighting the importance of testing both insulin and glucose levels for a comprehensive assessment.
In people with prediabetes and type 2 diabetes, insulin resistance is the most common underlying cause.
Why Is Testing for Insulin Resistance Important?
Standard diagnostic tests for diabetes, such as fasting glucose or an oral glucose tolerance test, focus on blood sugar levels.
However, it is possible to have normal blood glucose levels while exhibiting significant insulin resistance.
Identifying insulin resistance early allows you to adopt lifestyle and nutrition interventions that can prevent or delay the onset of type 2 diabetes.
A case study illustrates this point: a patient with normal fasting glucose but a fasting insulin level of 16 mIU/L, indicating moderate to severe insulin resistance, was on a trajectory toward type 2 diabetes. With proper intervention, such trends can be reversed!
Blood Tests for Insulin Resistance
To assess insulin resistance, discuss the following blood tests with your doctor, which they will order via pathology:
- Fasting Blood Glucose Test: Measures blood sugar levels after an overnight fast. Normal fasting glucose is typically less than 100 mg/dL (5.6 mmol/L). Elevated levels may indicate prediabetes or diabetes.
- NOTE: In Canada, UK and Australia, normal fasting glucose is often set at 6.0 mmol/L.
- Fasting Insulin Test: This test measures fasting insulin levels. Elevated fasting insulin can indicate insulin resistance, even when glucose levels are normal.
- HOMA-IR (Homeostasis Model Assessment of Insulin Resistance): This calculation uses fasting glucose and insulin levels to estimate insulin resistance. It offers a more accurate assessment compared to using fasting insulin levels alone.
- The formula is:
- Glucose (mg/dl) x Insulin mIU/L // (divided by) 405
- Glucose (mmol/l) x Insulin mIU/l // (divided by) 22.4
- NOTE: You won’t have to calculate this formula yourself, as the result will usually be indicated on your pathology report.
- HOMA-IR Insulin Resistance Test Range: There is no universally agreed-upon cut-off for HOMA-IR because “normal” values vary based on factors such as ethnicity, age, and obesity rates. However, general ranges used in research and clinical settings include:
- HOMA-IR <2.0 is excellent
- HOMA-IR 4.0 is average
- HOMA-IR above 4.0 is cause for concern
Interpreting Fasting Insulin Test Results
While HOMA-IR provides a more detailed analysis, fasting insulin levels alone can offer insights into insulin resistance status.
There are two units that can be used to express insulin concentration, 1 μU/mL = 1 mIU/L. These are both the same, but the unit on your report may differ depending on your location.
- 10 mIU/L or lower: Ideal, good insulin sensitivity
- 11–14 mIU/L: Mild insulin resistance
- 14 mIU/L: Moderate insulin resistance
- Over 20 mIU/L: Abnormally high insulin levels, strong insulin resistance
It is important to note that while these tests are valuable, they should be interpreted within the broader context of your individual medical history and risk factors.
Risk Factors for Insulin Resistance
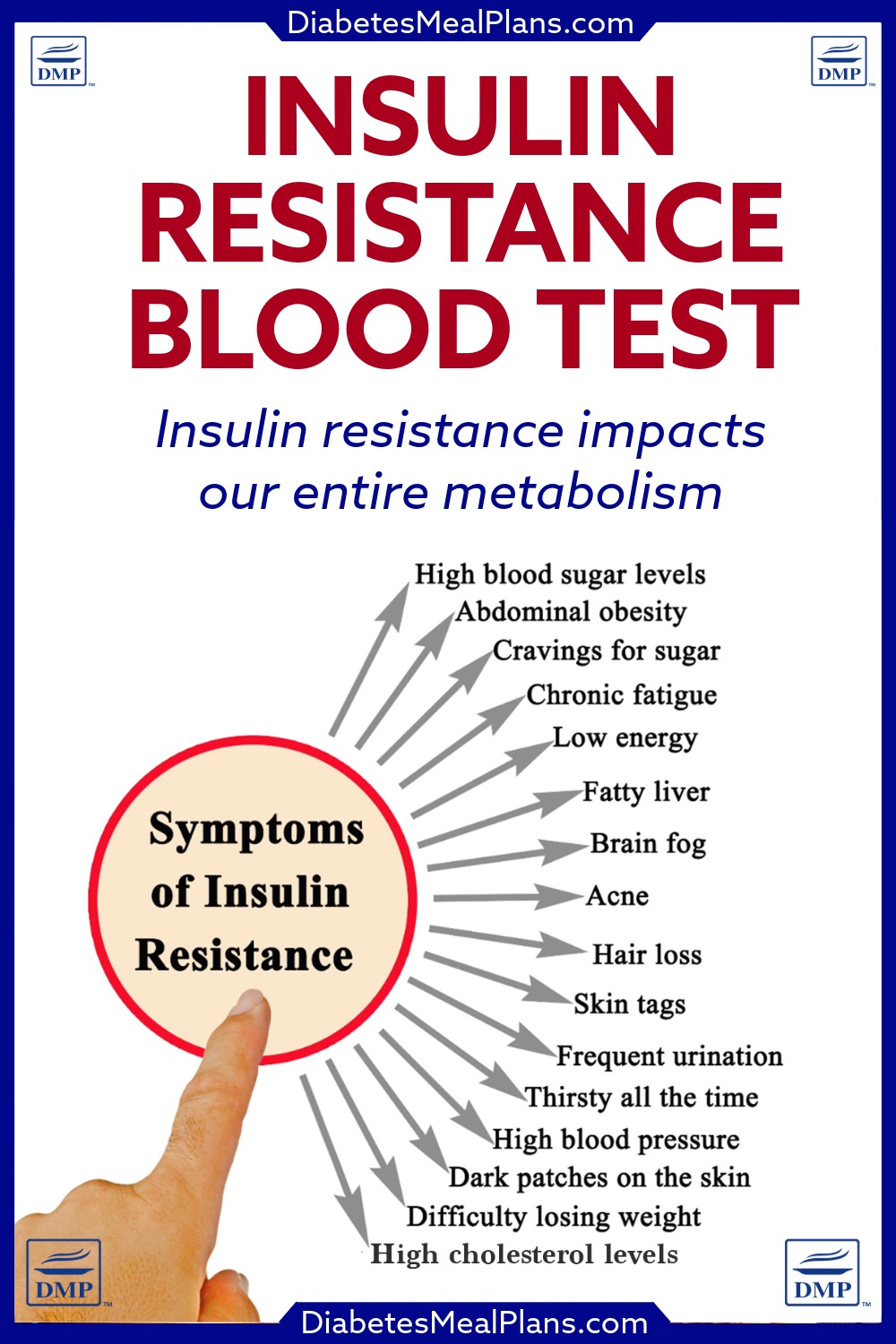
Several factors increase the risk of developing insulin resistance, including:
- Anthropometric Indicators:
- Body mass index (BMI) >25
- Waist circumference >40 inches or 101 cm (men) or >35 inches or 88 cm (women)
- Demographics:
- Age >40 years
- Certain ethnic backgrounds
- Health History:
- Family history of type 2 diabetes or cardiovascular conditions
- History of gestational diabetes or polycystic ovary syndrome (PCOS)
- Acanthosis nigricans (darkened patches of skin)
- Metabolic Markers:
- High blood pressure
- Elevated triglycerides
- Low HDL cholesterol
The Importance of Early Detection and Lifestyle Intervention
Detecting insulin resistance early allows you to implement lifestyle changes that can significantly reduce your risk of developing type 2 diabetes.
Evidence-based interventions include:
- Dietary Adjustments:
A low-carbohydrate, nutrient-dense diet has been shown to improve insulin sensitivity and reduce fasting insulin levels. - Physical Activity:
Regular exercise, including resistance and aerobic training, enhances insulin sensitivity by improving glucose uptake in muscle tissue. - Weight Management:
Reducing visceral fat (the fat around the belly/midsection) is critical, as abdominal obesity is closely linked to insulin resistance. - Stress Reduction and Sleep:
Chronic stress and poor sleep can worsen insulin resistance. Strategies such as mindfulness meditation and prioritizing sleep are beneficial.
The Value of Testing Insulin Resistance in Prediabetes and Type 2 Diabetes
Testing for insulin resistance is particularly valuable, even when you already have prediabetes or type 2 diabetes.
For those with prediabetes, identifying your level of insulin resistance provides an opportunity to intervene before blood sugar levels escalate further.
It allows for targeted lifestyle changes, such as dietary adjustments, increased physical activity, and weight management, that can help you reverse prediabetes.
For those with type 2 diabetes, understanding insulin resistance can help tailor your treatment strategy.
For example, if you know your insulin resistance level is moderate-to-high, you can focus on strategies that improve insulin sensitivity, rather than solely addressing blood sugar levels.
Regular monitoring of insulin resistance can also provide valuable feedback on the effectiveness of any strategies you put in place, ensuring that the focus remains on addressing the root cause of the condition rather than just its symptoms.
Next time you visit your doctor for an A1c test, request a fasting insulin test as well.
Conclusion
Insulin resistance is an invisible but reversible condition that often precedes prediabetes and type 2 diabetes, often by years.
Testing for insulin resistance, including fasting glucose, fasting insulin, and HOMA-IR, provides a comprehensive view of metabolic health.
Testing fasting insulin is incredibly important to assess insulin resistance, but it’s a test the doctor doesn’t usually test for, so be sure to ask for it.
By understanding your risk and taking proactive steps, you can significantly reduce your risk of developing prediabetes or type 2 diabetes.
Early detection empowers you to take control of your health, making insulin resistance testing an invaluable tool in preventive healthcare, and ensuring you maintain optimal health, over the long term.


my endocrinologist got upset when i mentioned i wanted to work on overcoming IR and would not order ANOTHER FASTING INSULIN TEST. he only wants use trulicity and invokamet xr to deal with my a1c……….i fear that trulicity may work against lowering my fasting insulin but cannot find anything in the literature on the subject…my fasting insulin is 16.5 and my c peptide is 3.4 and my a1c is 5.3 with a low carb diet. he repeatedly tried to keep a brick on my head saying that i should simply follow his instructions and he put down my efforts. i am 77 yrs old 215 lbs and 6′ 1″. i have decided not to return to that dr. again. can you comment on my assumption and tell where i might be able to order labs on my own…???
Hi Brian,
I cannot speak to the your questions regarding trulicity, but I would suggest finding another endocrinologist that listens to your concerns and is willing to order the tests you are interested in.
my mother is diebatic type 2 ..her blood sugar level is too much high ..she took medicine and also insulin 20 points..but still not progress..i am so worried please tell me what can i do
Hi Hina,
I’m sorry to hear about your mother’s difficulty with diabetes. Since I don’t know anything about her medical history I would urge you to visit her endocrinologist and express your concerns.
PS. I’ve shared your notes from https://diabetesmealplans.com/diet-to-lower-blood-sugar-a1c/ with the chief diabetologist and chief endocrinologist at the major teaching hospital here in Kathmandu and I’ll be copying at least part of that to share with their staffs next week, with due attribution to your website, if that is OK with you. Thank you for the clear, concise summary of research (with references) that you provide there.
Absolutely feel free to share, Jon.
Wow, you actually answered! I’ll be at the Nepali Health Research Summit mid-week and may find some answers there as well. I very much look forward to your response when you get more time to write. Thank you! Jon
I sincerely appreciate your thorough information on insulin resistance. I would love to receive help to get to the root cause of type 2 diabetes. WEARIED 😩
Glad you found the info useful Rene. If you’re feeling wearied and would love to receive help, please join us as a member – we provide you with lots of real support to get to the root cause and make life easier!
Dear Jedha,
We very much appreciate this article and the clarity it gives for testing IR using the HOMA-IR test. We’ve also seen a HOMA-Beta test for beta cell function. However this is more of a question or three than a reply.
Dr. Ede noted a formula for determining insulin resistance: the natural log of [(our fasting blood glucose x fasting triglycerides) divided by two]. Do you know if this is a reliable formula? Do you have a formula by which we could substitute HbA1C for the fasting blood glucose (fbg) ?
I think that HbA1C would be a much more reliable number here in Nepal, where diabetics typically have their fbg taken once a month. However, a serum insulin test for the HOMA-IR calculation costs a common laborer almost three days wages ($12.60), whereas a fasting triglyceride test is five times less ($2.65) (and HbA1C is $7.35).
We are planning a research project here to measure the Insulin Resistance response to Intermittent Fasting (IF) and a Low Carb (LC) diet. We see IR as a major contributor to several chronic diseases that are rapidly increasing in Nepal, including obesity and T2 diabetes. Therefore we want an affordable but accurate way to measure it. [My wife is a T2 and a former nurse who for over four years has been managing her diabetes using a LC diet and more recently (and effectively) IF and by the fbg/ftg calculations, her IR has dropped dramatically recently.] Hopefully this will provide a local evidence base for using a dietary approach to address IR in a Nepali cultural context. We may need to do some groundwork first since IF is mostly unknown here. If anyone on your staff is interested in working with us, or critiquing our efforts, we also would be very appreciative of that.
With thanks,
Jon and Diane
Hi Jon – thanks for your questions and interest in working with us on your research project. I will send you an email soon to discuss this more, but it may not be for around a week as I will be away. Talk soon.