If you define cure as it’s most commonly understood: “a healing or remedy by which health is restored,” then in all accuracy, weight loss is not a “cure” for type 2 diabetes. That is, there is no remedy that will resolve the disease itself.
However, while diabetes is not reversible from a diagnostic standpoint (once you have it, you have it), diabetes can be reversible from a physiological standpoint in many.
That is, you can work to get your blood glucose within a normal healthy range, maintaining glucose control so you are functioning like a non-diabetic.
So, while there is no “cure” per se, that doesn’t mean there aren’t a multitude of “treatments” that you can apply to improve symptoms, reduce risk and sometimes reverse physiological trends. And weight loss can be one of those “treatments” that can help.
Let go of the ‘quick fix’ mentality
You have to be careful. Looking for a “cure” can conjure up the kind of thinking that tends to gravitate along the lines of ‘quick fix,’ the same as we find in fad dieting in which you go ‘on’ something for a period of time to ‘fix’ the issue and can then go back “off” it and resume your previous pattern.
This happens a lot in the weight loss industry. And it’s something that gets us all in a trap in many instances, going around in circles for years on end. You know, you lose some weight, feel better, then go back to your old habits and bam…all positive effects achieved by weight loss will simply be thwarted once weight is regained. And you feel terrible because you ‘fell off the wagon.’

Lifestyle (and Weight Loss) Can Greatly Impact Type 2 Diabetes
While no one can guarantee complete hormonal restoration with diabetes, lifestyle changes may be able to slow, halt and reverse physiological function to some degree. In some cases, people can take fewer medications or even eliminate diabetes medications. Some can go into prolonged remission – so to speak.
Weight loss specifically has been shown to be one of the top risk factors associated with the development of type 2 diabetes. Obese people are at higher risk of almost every disease due to increased inflammation in the body and decreased immune function.
Weight loss specifically has been shown to be one of the most beneficial ways to reduce A1c and diabetes complications. Without a doubt, it’s fairly well-known that weight control reduces risk of heart disease and heart attacks, can lower high blood pressure, kidney failure, and so forth.
This is the foundation of the Diabetes Prevention Program. Their results were so staggering that insurance companies are reimbursing them for the people who participate in the program.
Here’s the great news: the weight loss doesn’t have to be extreme to see very good results. Reduction of only 5-10% of a person’s body weight resulted in reduction of risk (and risk of complications) by up to 60%!
As an example, if you weigh 200 pounds, that means 10-20 pounds is enough to really see your risk go down.
Understanding Insulin Resistance and Weight
Obesity is linked with insulin resistance. While it is estimated that about 32% of the US population is insulin resistant, that number climbs to 70% in the obese. Insulin resistance is a major contributing factor to the progression of type 2 diabetes because most people are still capable of making insulin, but the cells in their body have become resistant to insulin.
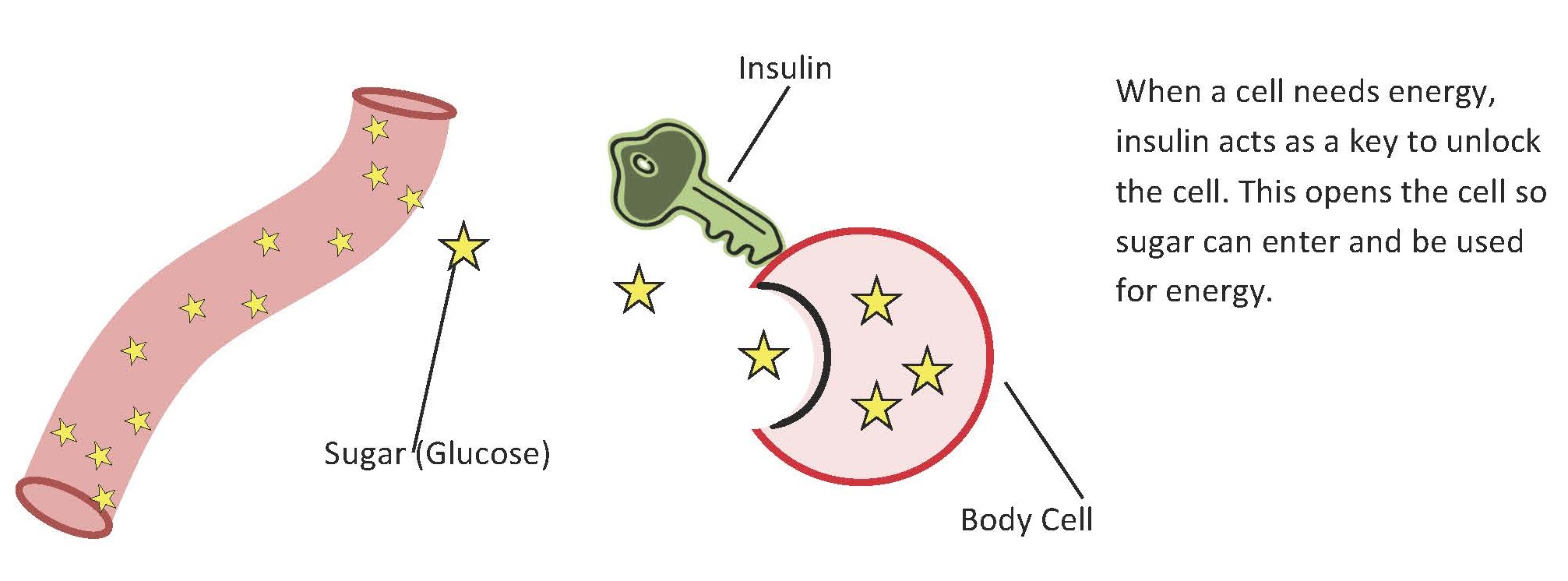
Insulin is the hormone that helps lower blood sugar. It’s the key that opens the cells. When you’re insulin resistant, your insulin isn’t unlocking the cells as efficiently.
Insulin resistance makes the pancreas work harder. So in many cases people can be hyperinsulinemic – have too much insulin production – high insulin levels. The pancreas tries to make more insulin, trying to get the glucose out of the blood into the cells.
If it has to go on like this for some time, eventually it gets tired and starts pooping out. Sometimes exogenous (injectable) insulin is needed to make up for the difference.
Mounding evidence shows that what likely happens is that the excess fat buildup around the tissues (in the liver and belly fat) interferes with the cell receptors so that insulin isn’t able to do it’s job properly. So, glucose ends up hanging out in the bloodstream, causing damage to cells and not getting into the cells where it is needed to do it’s job.
Losing Weight Improves Insulin Sensitivity
When people lose weight, they often decrease their insulin resistance and in turn make their cells more sensitive (insulin sensitivity), needing less insulin over time and preserving what is left of their pancreas function.
The effect is more prominent in those who are more obese, but anyone, even those in the overweight category will benefit from some weight loss.
Body Mass Index, otherwise known as BMI is often used as a guideline for ideal weight because in most scientific studies it still serves as a good reference point for health.
To find out what your BMI is, check out this calculator.
Simply plug in your information and it will tell you where you currently fall on the spectrum and what your target levels are.
- A BMI between 18.5-24.5 is considered a healthy weight range.
- Between 25-29.5 is overweight
- Over 30 is obese.
Keep in mind this calculation only takes into consideration height and weight, not frame size, body fat percentage or other factors. But it’s a great start to get an idea as to where you stand.
How To Lose Weight: 5 Practical Tips
Knowing that you should lose weight is much different than knowing how. And knowing how is very different than putting it into practice. Even when we know better, doesn’t mean we still do stuff, right?
Most of us know that weight loss will help. But understanding a bit more about it can be helpful by way of motivation and as a reminder. The nitty gritty part is putting it into practice -taking action. We can’t do that for you, but we can help you with the ‘how.’
Tip #1: Eating a healthy balanced diet is absolutely KEY to achieving weight loss.
Tip #2: Keep in mind that watching your total carbs and practicing portion control will help ensure you aren’t consuming excessive amounts.
Tip #3: If you need help with meal planning and calculating calories and carbs on a daily basis, check out our 4 week “smart” weight loss meal plan. It does all the calculations for you.
Tip #4: Work on curbing unhealthy habits like nighttime eating and making better choices when traveling or eating out.
Tip #5: Develop a regular exercise plan and be sure to work on healthy responses to stress, along with ensuring you get adequate sleep.
It is really key to cultivate a healthy long term mindset when it comes to all of this. Think of it as a permanent lifestyle change rather than “going on a diet,” which implies you’ll be doing it only for a short time. Instead strive for better daily habits by embracing tried and true healthy eating patterns known to be effective at sustaining well-being.
That’s one of the reasons this site exists – for people like you who are trying to cultivate this with like-minded folks. We’re a sort of support group for one another, providing resources, feedback and encouragement to help you on your journey.
So can weight loss cure diabetes?
Not cure, exactly. But…even a small amount of weight loss, 5-10% of your body weight, can improve, halt or reverse symptoms. So in some shape or form, it can in a sense help “cure” things.
The challenge for you is to start making better choices for yourself.
We’re here to support you and we know you can do this!
Need help to lose weight and lower blood sugar?


Brewster
Doubt that it Can be cured but surely managed. We were out on one of our infamous weekend nosh’s, it was pizza Saturday night. Had a coffee with St.Martin/Baileys then my glass of red wine a bit later. Sunday am my blood sugar was 4.5. Ah Monday, back to eating sensibly.
Elizabeth
You’re right, it can be managed and there are a lot of resources available to help you, this site being one of them!
James
It can be cured Jason Fung