If you want to improve insulin sensitivity, the first step is to evaluate your diet and lifestyle habits.
It’s here you’ll find the solution to prevent and reverse the consequences of being insulin resistant – namely, a change in glucose tolerance, which often results in higher than normal blood glucose levels.
If you’re prediabetic or already have type 2 diabetes, knowing how to improve insulin sensitivity is important, which is exactly why we’re going to cover this in detail right now.

Insulin Explained
Some people do become fearful even hearing the word “insulin” because it brings up scary associations.
But just remember that insulin is simply a hormone the human body naturally makes. And we need it to survive.
The hormone insulin is made by the pancreas and it’s job is to facilitate glucose uptake by moving the sugar from the bloodstream into the cells to be utilized for a variety of purposes, most significantly, energy.
If there isn’t enough insulin, or it isn’t working properly, sugar will build up in the bloodstream – or in other words, you’ll end up with high blood sugar.
With type 2 diabetes, insulin metabolism is altered.
A person with type 2 diabetes either has a system that:
- Does not accurately recognize elevated glucose, OR
- Is not producing enough insulin–what often happens is that poor glucose control causes an INCREASED production of insulin (hyperinsulinemia), which eventually leads to the beta cells (cells that make insulin) burning out and dying, OR
- (Most commonly) Cells become resistant to insulin, otherwise known as insulin resistance.
Insulin Resistance
Insulin resistance is a key metabolic factor that proceeds type 2 diabetes – meaning, it is present long before a person is diagnosed.
Therefore, if you’re prediabetic, you likely have insulin resistance. And once you have a diagnosis of type 2 diabetes, insulin resistance becomes an added challenge.
While your body can still make some insulin (though it may be less in some people), the bigger issue is that the body is unable to utilize the insulin correctly.
The cells in your body are “resisting” the work the insulin is trying to do and becoming “desensitized” to it. The body’s cells tune out to insulin and stop listening to it.
Picture insulin there at the door of the cell with the key, ready to bring in the glucose.
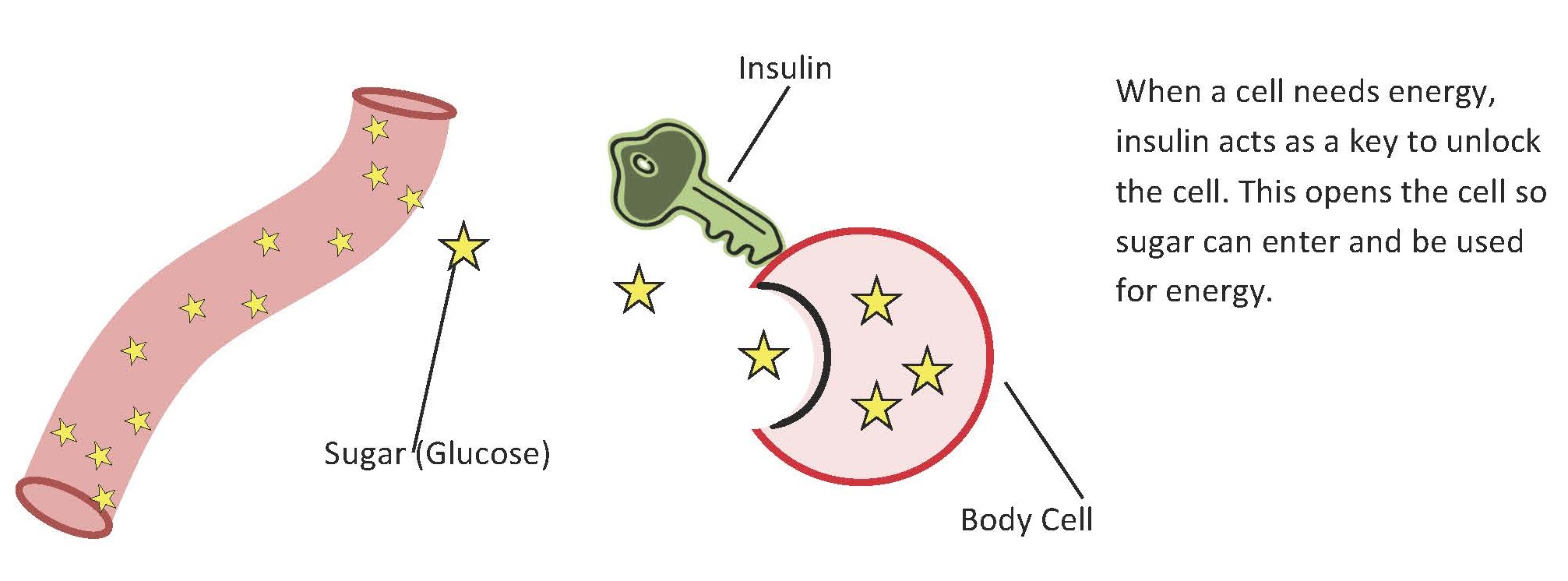
Under normal circumstances insulin unlocks the cell so that sugar/glucose can be moved out of the bloodstream and into the cells.
Now imagine the cell folding its arms saying, “nope, sorry, that key doesn’t fit anymore. I changed the locks.” That’s insulin resistance.
Rather than letting the glucose in, the cells no longer listen to the hormonal signals that are sent. So the more sugar that stays in the bloodstream, the more cells remain starved for energy.
As a result, the body tries to compensate by making more insulin – pumping more of it out from the pancreas to try to get those cells to unlock. But in many cases this doesn’t help. You simply end up with high glucose and high amounts of insulin circulating in the blood.
And unfortunately, high insulin levels are linked with:
- Blood vessel damage
- High blood pressure
- Heart disease
- Cancer
In addition, weight gain is likely because when the insulin does work, it stores whatever it can get hold of, as body fat.
So overall insulin resistance contributes to:
- Diabetes
- Obesity
- Heart disease
- Fatty liver
- And many other chronic conditions
If a person is insulin resistant, it will essentially evolve into type 2 diabetes if lifestyle changes aren’t made, and sometimes even when they are.
Insulin resistance is the result of metabolic syndrome and can result from a combination of both lifestyle and genetic factors.
Risk factors include:
- Obesity
- Sedentary lifestyle
- Poor diet
- Steroid use
- Illness/infection
- Stress
- Poor sleep
- Smoking
- Genetic factors
- Age
Insulin Sensitivity
Insulin sensitivity is the opposite of insulin resistance. It means that the body’s cells are very perceptive and responsive to the insulin signals produced.
While we don’t want to be overly sensitive to insulin, which can cause hypoglycemia very easily, for most of us, that isn’t a problem. Really, for a person with type 2 diabetes or prediabetes, improving insulin sensitivity is your goal because it reduces your insulin resistance and improves the efficiency of the cells to take glucose – it helps that insulin key unlock those doors.
Insulin sensitivity can be measured by a blood test to detect circulating insulin, although doctors rarely order this test because treatment for high blood sugars is really the same anyway.

Ways to Improve Insulin Sensitivity
While we can’t stimulate our bodies to make more insulin, we can make lifestyle changes that help improve sensitivity to insulin. This is where the terms “prevention” and “reversal” can hold true for many.
If you’re insulin resistant/ prediabetic, you can prevent a type 2 diabetes diagnosis by improving your insulin sensitivity, thereby decreasing your insulin resistance and promoting better metabolic health and function.
If you have type 2 diabetes, you can reverse your insulin resistance and improve glucose control by increasing your insulin sensitivity.
And there are a range of lifestyle changes that can help you do this.
Weight Loss
Weight loss is one of the most effective ways to reduce insulin resistance/improve insulin sensitivity.
Prediabetes is the result of insulin resistance in 58-71% of people. The more weight a person carries, the more cells demand energy and the less effective insulin is at doing it’s job.
Weight gain in the abdominal region (aka belly fat), surrounding central organs, increases risk even further. So if you are overweight or obese, set a realistic goal of 0.5-2 pound (0.25-1 kg) weight loss per week.
Research shows that as little as 5-7% weight loss can improve insulin sensitivity enough to ward off a diabetes diagnosis in people with prediabetes. And if you sustain the weight loss, research shows you’ll also sustain your insulin sensitivity long term.
In people with diabetes, reducing weight not only helps to re-sensitize the body to insulin but it improves other biomarkers such as cholesterol, inflammation, blood pressure, and glucose control.
Exercise
Exercise demands glucose, which means physical activity will place greater demand on the cells in the muscles to respond to insulin.
In fact, moderate activity can improve insulin sensitivity in as little as a few days!
Obviously consistency over the long term will yield the best results. So it really is recommended that you engage in at least 30 minutes of exercise each day – both aerobic activities along with strength-based activities.
Walking tends to be the easiest, most cost effective thing for people to do. And strength/ resistance exercises that use the large muscle groups in the legs are very effective – for increasing muscle mass, improving fat burning potential, and improving insulin sensitivity.
Resistance training exercises might include:
Check out this info for a more thorough description of exercise for type 2 diabetes.
Healthy Diet
Eating a healthy diet is a given. But one of the many reasons we advocate avoiding high carbohydrate and high glycemic index foods is that they require more insulin to process. A higher carb intake requires more insulin. And remember when there is more insulin, this drives up insulin resistance.
Lowering the amount of carbs you eat, means less glucose in the bloodstream, less insulin and therefore, improved insulin sensitivity.
Avoid sugars, white flours and white foods, which spike blood sugar causing demand for more insulin. Avoid higher carb foods such as potatoes, pasta, rice, and bread – even the whole grain type, as they are still high in overall carbs and will demand more insulin.
And while fruit is healthy, it has a higher glycemic index compared with vegetables, so be cautious with portions and always try to eat some form of protein along with it. Berries are really your best fruit option overall.
Aim to include lots of non-starchy vegetables, lean protein, healthy fats – that makes up a healthy low carb diabetic diet!
Medication
Some medications improve a person’s sensitivity to insulin. For instance, metformin and GLP-1s (ie Byetta and Victoza) are both effective at improving sensitivity to insulin.
Keep in mind that some medications can have the opposite effect – increasing blood sugar and demanding more insulin.
This is especially true in the case of steroids, which are often taken to control pain. Be sure to discuss your whole medication regimen with your doctor to ensure you aren’t taking anything unnecessarily that might increase glucose.
Supplements
There are many supplements available that may help improve the body’s sensitivity to insulin.
For instance:
Milk thistle: Helps improve insulin sensitivity by working on a fatty liver.
Berberine: Helps lower blood sugar levels and aid weight loss, which subsequently helps improve insulin sensitivity.
Cinnamon: May help improve glucose utilization and insulin function.
Fish oil: Reduces insulin resistance and improves insulin sensitivity, perhaps by driving down inflammation in the body.
That’s just a few examples. Remember though, that supplements are not regulated by the FDA and overall, while there is research to show their effectiveness, we still need more research to prove their effectiveness conclusively.
Make sure you discuss any supplements you are considering taking with your doctor and pharmacist to make sure there aren’t any contraindications.
Overall though you can see that there are many habits you can change that will improve your insulin sensitivity. And of course, the more you can do, the better your metabolic function will get as well.
Please pin, tweet or share this info to help others. Thanks!

Barbara Funderburg
Just checking in. Great article.
Rhonda
Thanks for the info, FS 158 this morning – not good
Virginia
Checking in.
Great article
Malorie: Dietitian (MS, RD, CLT)
Thanks for checking in Virginia!
Ginger
Day 15 and my Fbs a.m. remained the same as yesterday …
I so appreciated the in depth article of information in understanding of improving insulin sensitivity/ resistance, this help immensely as well as the uses of the supplements…
Blessings
Ginger
Malorie: Dietitian (MS, RD, CLT)
Glad the information has been helpful to you! Thanks for checking in.
Robert Cooper
Best explanation I have ever seen and fully understandable. Well done. Many thanks.
laurie wilson
can you use metformin and berberine together
Jedha: Nutritionist (MNutr)
Yes you can but should consult your doctor about any supplementation. Research studies have shown that combined therapy can improve fasting glucose and A1c. Thanks for checking in Laurie.
Marlene
at bedtime last night BS 7.4 and this morning it was 8.4.
I am trying to eat more veg. I cooked cauliflower in the steamer yesterday and it was delicious. Nice and crunchy. This morning for breakfast I had leftovers from supper – steak, green beans and cauliflower. No food cravings all morning!
Jedha: Nutritionist (MNutr)
Good to hear Marlene – keep up that commitment. ;)
lynda
I have really learned a lot about diabetes just from your site. my mother had diabetes ,she pased in the 70’s and i have always felt guilty cause i did’t know much about this disease.even today it amazes me that people are not informed.thank you .I have tried some of the recipes and thanks again .I was so frustrated about what to make for meals.keep doing what your doing.
Jedha: Nutritionist (MNutr)
Thanks for your kind words Lynda. Glad everything is helping. :)
Kelly Wilson
Never really understood insulin sensitivity so this was so helpful. Thank you. Numbers are still doing well so now I’m hoping to continue working towards better health. Thank you so much! Great info!!
Jedha: Nutritionist (MNutr)
Glad you’re enjoying it Kelly. Thanks for checking in.
Tina Falconer
129 before bed, but 190 FBS this morning – why?
Jedha: Nutritionist (MNutr)
Did you check out the info on fasting blood sugar Tina – will explain why this may happen.
Gerry
Great article. Thank you! Need to read several times so this concept really ‘sinks’ in. You explain it very well and simply.
Emily - Dietitian (MS, RD)
Thanks for the positive feedback!
Margaret
Very informative article. I have spent this am reading articles in the library section. I have found answers to many questions that I have had for years.
Ellen
Checking in.
Kept to my plan. going good
Malorie: Dietitian (MS, RD, CLT)
Glad everything is going well-thanks for checking in!
Carol
FBS 135 Thank you for your comments about snacks and carbs. Today’s article about improving insulin sensitivity was helpful.
Bill
This is a great article and broken down for me to grasp. It reminds me of signs in my past (fatty liver deposits) 20 years prior to being termed a T2 diabetic. With those findings I did not receive any help from medical professionals until I had a very old type 2 PA that told me try 4 oz servings of fish, turkey, or chicken accompanied by green leafy veggies, only. Once I took his advice my AST dropped from 124 to 75 and my ALT dropped from 132 to 41 (within range)
Jodi
Great article about resistance.
FBS today 151
MARY
I am 74 year female and was diagnosed with type 2. I have not been able to locate a dietitian in my area. A RN at Dr office with some knowledge gave me a sample menufor one day. This came from the ADA, it suggested I eat 30 grams of carbs per meal and snack. This is way too much for me. Could you help me please?
Jedha: Nutritionist (MNutr)
Hey Mary, 30 grams per meal is pretty high, ADA guidelines have always been steep – at least they’ve come down from the 45 grams they were recommending just a year ago! This info here might be useful.
Susan Lim
Thank you so much for sharing such an enlightening article!
Lori
Great article! Thanks for the inspiration!
Abeer
Thank you so much, I really appreciate sharing such an informative article.