Table of Contents[Hide][Show]
When navigating perimenopause or menopause with type 2 diabetes or prediabetes, it can contribute additional challenges that you need to think about.
Or if you’re a woman going through perimenopause or menopause and wondering how it influences blood sugar, you’re in the right place.
This time of life can bring unique challenges, especially when it comes to balancing blood sugar.
But there is good news: understanding the connection between menopause and blood sugar can empower you to take meaningful steps toward better health.
Let’s explore how menopause affects blood sugar, why these changes occur, and—most importantly—what you can do about it.
LISTEN TO THE PODCAST
CHAPTERS
2:23 The menopause transition
4:18 Menopause and blood sugar
6:37 Sarcopenia, metabolism and bone loss
11:34 Nutrition for menopause and diabetes
19:55 Essential nutrients during menopause
Support the podcast by leaving a 5-star rating and review on Apple, Spotify or our Website – Thank You!
How Menopause Affects Blood Sugar
During menopause, your hormone levels—particularly estrogen and progesterone—fluctuate and eventually decline.
These hormones don’t just regulate your menstrual cycle; they also play a critical role in how your body processes glucose.
Insulin Sensitivity
Insulin is a key hormone that helps regulate blood sugar levels. We want to keep our insulin sensitivity high, so that insulin can perform it’s job properly.
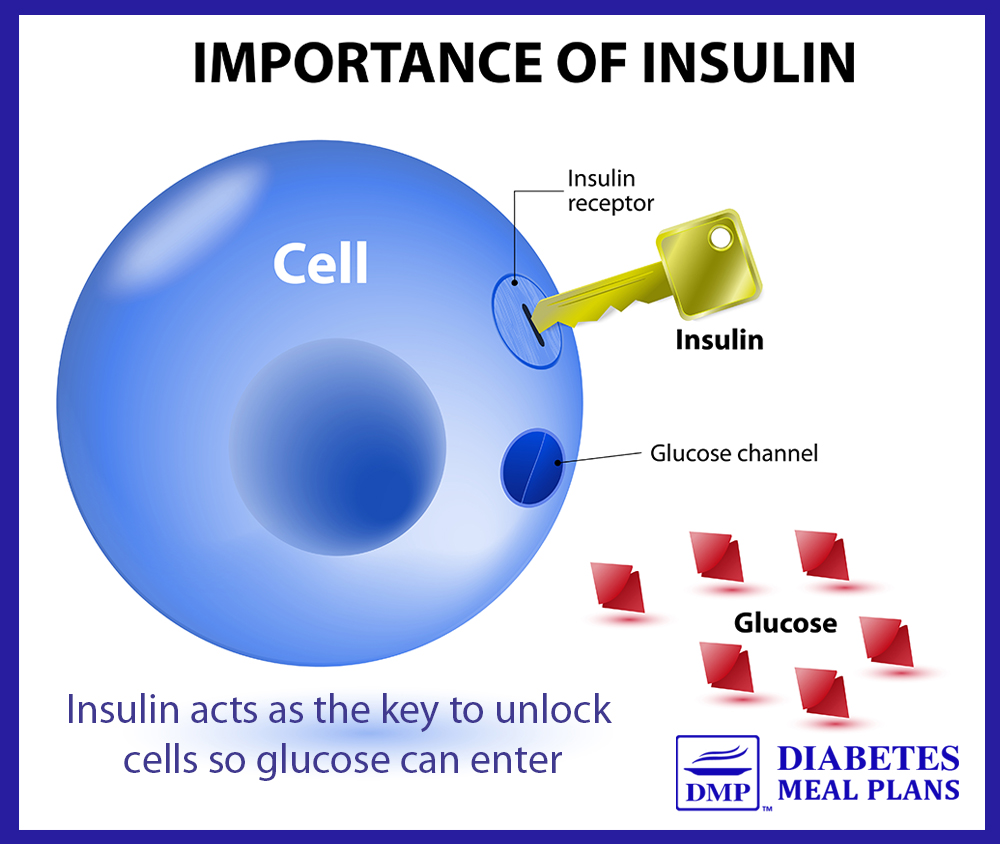
Estrogen has a protective effect on insulin sensitivity. When estrogen levels drop, your body may become less responsive to insulin, making it harder for glucose to move out of your bloodstream and into your cells.
This is known as insulin resistance, which can result in higher blood sugar levels.
Fat Distribution and Weight Gain
Menopause often brings a shift in fat storage, with more fat accumulating around the abdomen.
This type of fat, called visceral fat, is metabolically active and can increase insulin resistance, further driving up blood sugar levels.
Sleep Disruptions
Menopausal night sweats and hot flashes can make restful sleep feel like a distant dream. During perimenopause, you may also notice sleep disruptions due to fluctuating hormone levels.
Poor sleep is linked to insulin resistance, weight gain and higher fasting blood sugar levels, making it harder to stabilize your glucose levels during this transitional phase.
Stress and Cortisol
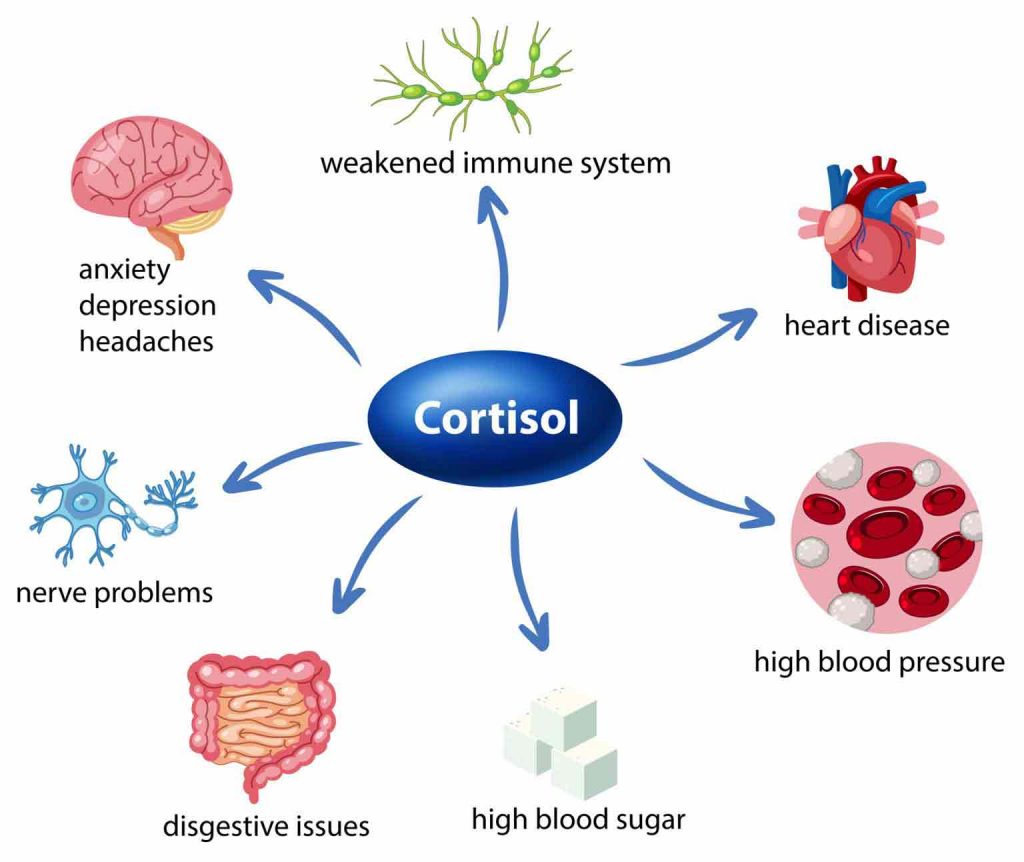
Hormonal changes during menopause—and even earlier, in perimenopause—can heighten stress levels and increase production of cortisol, a stress hormone.
Elevated cortisol not only raises blood sugar but can also exacerbate insulin resistance, creating a cycle that impacts energy levels and mood.
Learning to manage stress during this period is a crucial part of balancing blood sugar.
Perimenopause and Blood Sugar: Early Changes to Watch For
Before menopause, most women go through perimenopause, the transitional phase where hormone levels fluctuate unpredictably.
These fluctuations can start as early as your late 30s or 40s and can last several years. They also impact blood sugar regulation in several ways:
- Estrogen Fluctuations: When estrogen dips, insulin sensitivity drops.
- Progesterone Spikes: Higher progesterone levels can temporarily worsen insulin resistance, leading to blood sugar spikes.
- Increased Cravings: Many women report cravings for sugary or starchy foods during this time, which can affect blood sugar control.
Addressing blood sugar imbalances early during perimenopause can help ease the transition into menopause and reduce your risk of long-term complications.
Common Blood Sugar-Related Symptoms During Perimenopause
You might notice subtle changes in your blood sugar control during perimenopause, such as:
- More frequent blood sugar spikes or crashes, especially after high-carb meals.
- Increased sugar cravings or cravings for starchy foods.
- Difficulty losing weight or unexplained weight gain, particularly around your midsection.
- Greater fatigue or brain fog after meals, linked to unstable blood sugar.
Why Menopausal and Perimenopausal Changes Matter
The shifts in blood sugar control during menopause and perimenopause can increase your risk of complications if left unaddressed.
These include:
- Higher blood sugar and A1c levels
- Difficulty managing weight
- Increased risk of cardiovascular issues
But here’s the key takeaway: these changes are not inevitable.
By understanding how perimenopause and menopause affect your blood sugar and taking proactive steps, you can improve your health and well-being during this time of life.
Why It’s Important to Act During Perimenopause
If you can, addressing blood sugar imbalances during perimenopause can set the foundation for better health as you transition into menopause.
Proactively managing your blood sugar now can reduce the risk of developing type 2 diabetes, heart disease, or other metabolic issues later.
Steps to Balance Your Blood Sugar During Menopause and Perimenopause
Whether you’re currently living prediabetes or type 2 diabetes, or you’re a woman concerned about how perimenopause or menopause may affect your blood sugar, the good news is there are proven strategies to help you take control.
1. Optimize Your Nutrition
What you eat plays a pivotal role in managing both menopause symptoms and blood sugar levels.
Focusing on a quality nutrition plan is going to be the most important thing for balancing blood sugar, keeping the weight off and staying in optimal health.
Prioritize Protein
Protein helps stabilize blood sugar by slowing the absorption of carbohydrates and keeping you feeling fuller longer.
Aim to include high-quality protein sources like eggs, chicken, fish, and plant-based options such as soybeans, tofu or lentils with each meal.

Eat Tons of Vegetables
Vegetables are the best type of carbohydrate to eat, as they are lower in overall carbs, contain fiber and powerful antioxidants and polyphenols that can help reduce inflammation and balance blood sugar.
Incorporate Healthy Fats
Healthy fats from sources like avocados, nuts, seeds and olive oil can reduce inflammation and support insulin sensitivity.
Overall, you really need to have a clean diet, a quality nutrition plan that will help you address the issues that come with perimenopause or menopause.
Your nutrition plan is going to be one of the most important things to focus on.
2. Move Your Body Regularly
Exercise is one of the most effective tools for improving insulin sensitivity and reducing blood sugar levels. It’s really important to move your body more. But exercising smart is key.
Strength Training
During perimenopause and menopause women lose muscle mass, so including strength training can lead to better results.
Building muscle can help you lose weight, plus, it enhances your body’s ability to use insulin effectively.
Aim for strength exercises 2-3 times a week.
Aerobic Exercise
Alongside strength training, try to include regular aerobic exercise.
Activities like walking, cycling, or swimming help improve glucose uptake by your muscles. Even a brisk 10-minute walk after meals can make a difference.
Tip: Consistency matters more than intensity. Start with activities you enjoy and gradually build from there.

3. Prioritize Sleep
Prioritizing sleep can’t be emphasized enough: You absolutely need quality sleep during perimenopause and menopause.
While we know sleep can be disrupting at this time, do the best you can to get better sleep, as this will lead to better blood sugar control.
Here’s a few tips:
- Establish a Routine: Go to bed and wake up at the same time each day, even on weekends.
- Create a Cool, Dark Sleep Environment: Lowering the temperature and using blackout curtains can help combat night sweats.
- Limit Caffeine and Screens: Avoid both at least two hours before bed to promote restful sleep.
4. Manage Stress
As mentioned above, chronic stress raises cortisol, which can disrupt blood sugar levels.
- Mindfulness Practices: Deep breathing, meditation and yoga can reduce cortisol levels and improve insulin sensitivity.
- Time in Nature: A simple walk in a green space can lower stress and blood sugar levels.
- Support Network: Don’t hesitate to reach out to friends, family or a counselor when you need support.
Tip: Experiment with stress-relief techniques to find what works best for you.
5. Monitor Your Blood Sugar
Monitoring blood sugar can help you understand how your body responds to different foods, activities and stressors.
- Use a Glucometer: Check your blood sugar before and after meals to see how your choices impact your levels.
- Consider a Continuous Glucose Monitor (CGM): A CGM provides real-time insights into your blood sugar trends.
6. Incorporate Adaptogenic Herbs
Adaptogenic herbs, such as ashwagandha, maca root, and rhodiola can provide perimenopause and menopause support.
For example, ashwagandha has been shown to reduce stress and lower cortisol levels, potentially improving insulin sensitivity.
Maca root may support energy and mood during perimenopause and menopause, helping you stay motivated for healthy lifestyle changes.
Rhodiola, on the other hand, is known for its ability to reduce fatigue and improve resilience to stress, both of which can help with overall blood sugar management.
Post-Menopause and Blood Sugar: What to Expect
After menopause, once your hormone levels have stabilized at lower levels, blood sugar regulation remains a critical focus.
The absence of estrogen’s protective effects can make it more challenging to maintain insulin sensitivity and manage your blood sugar effectively.
Here’s what you need to know about the post-menopausal phase.
Why Post-Menopause Matters for Blood Sugar
During post-menopause, women often face compounded metabolic challenges due to:
Persistently Low Estrogen Levels
Estrogen plays a key role in supporting insulin sensitivity and keeping glucose levels stable.
Without estrogen, the risk of developing insulin resistance increases, potentially leading to higher blood sugar and A1c levels.
Body Composition Changes
The accumulation of visceral fat around the belly—common in post-menopause—can worsen insulin resistance, inflammation and overall metabolic health.
Even if your weight doesn’t change, shifts in fat distribution may increase blood sugar instability.
Higher Cardiovascular Risk
The metabolic shifts during post-menopause can elevate your risk of heart disease, especially when paired with poor blood sugar control.
Keeping blood sugar stable becomes even more crucial for protecting your heart health.
Bone and Muscle Health
Declining estrogen can also lead to reduced bone density and muscle mass.
Since muscle is one of the body’s main sites for glucose uptake, maintaining strength is vital for managing blood sugar.
Proactive Strategies for Post-Menopause
The good news is that with the right approach, you can still support healthy blood sugar levels and reduce risks of complications in the post-menopausal years:
1. Strengthen Your Muscles
- Prioritize resistance training to maintain muscle mass and improve insulin sensitivity. This is especially important as muscle naturally declines with age.
- Incorporate weight-bearing exercises like walking or yoga to support both blood sugar and bone health.
2. Focus on Anti-Inflammatory Foods
Post-menopause often brings more systemic inflammation, which can worsen insulin resistance.
Combat this with anti-inflammatory foods, such as:
- Fatty fish (salmon, mackerel, sardines) for omega-3s.
- Berries, leafy greens, and cruciferous vegetables like broccoli and cauliflower for antioxidants.
- Healthy fats like olive oil, nuts and seeds.
3. Address Fat Redistribution
If abdominal fat is becoming a concern, focus on reducing visceral fat through:
- Intermittent Fasting: Focusing on meal timing, such as eating breakfast later, can improve insulin sensitivity and help with fat loss.
- Portion Awareness: Avoid overeating even healthy carbs like whole grains or starchy vegetables.
- HITT: Incorporate High Intensity Interval Training, which includes short bursts of intense activity followed by recovery periods—can help women at all stages of menopause manage body composition, particularly abdominal and visceral fat, while improving overall metabolic health.
- Afternoon Exercise to Increase Fat Burning: Research indicates that training in the afternoon can help burn more fat, so workout in the afternoons to maximize your exercise outcomes.
Menopause: Moving Forward With Confidence
Perimenopause and menopause bring changes that can make managing blood sugar more challenging, but they also offer an opportunity to take charge of your health.
While post-menopause brings lasting hormonal changes, it also offers an opportunity to build a long-term plan for optimizing your health.
By focusing on optimizing your nutrition, regular exercise, stress management and good quality sleep, you can significantly improve your blood sugar control during this transitional time.
With the right strategies, you can navigate this phase of life with confidence and enjoy improved health and well-being well into your later years.
Transcript
Click Here To View
Dr Jedha, Host
Hello wonderful ladies and thanks for tuning into today’s episode, which comes in honor of Women’s Health Week. And I’m excited to talk about today’s topic, because it’s something incredibly important for all of us women, and that is, how hormonal changes from perimenopause to post-menopause affect our blood sugar.
For those of us navigating perimenopause, menopause, or post-menopause, and especially when managing type 2 diabetes or prediabetes, these hormonal shifts can bring unexpected challenges.
Maybe you’ve noticed weight gain around the midsection that wasn’t there before, or cravings that feel stronger than they used to. Perhaps fatigue or brain fog hits you after meals, or sleep disturbances leave you drained and frustrated. Maybe you’ve experienced bouts of depression, headaches or migraines that you never suffered from previously. What many women don’t realize is that these changes can be traced back to how estrogen, progesterone, and insulin interact.
By understanding how these shifts affect us as women, we can take proactive steps to reduce symptoms and support our long-term health.
02:23
For most women, perimenopause typically starts in the mid 40s and can last several years. Most women know they’ve entered this early menopausal transition because the menstrual cycle changes and there is often a 7 day difference in cycle length of consecutive cycles. During this time, our hormone levels can take us on a bit of a roller coaster ride. Hormones like estrogen and progesterone can fluctuate unpredictably. One day, we might have higher estrogen, and the next day, it could drop dramatically. This is what creates that rollercoaster effect that many of us feel.
When we reach menopause, which for many women happens in our 50s, our bodies stop producing as much estrogen and progesterone, and we stop having periods. When our period stops for an interval of 60 days or more, then we’ve entered the late menopausal transition.
Early postmenopause occurs when 12 months have passed since the last period. Once we’re past menopause, our hormone levels stabilize, but they’re at consistently lower levels than before.
Through this transition period it can be a difficult roller coaster, due to the changes in hormones that are occurring in our bodies, estrogen has protective and regulatory effects on our metabolism, so when our estrogen levels get lower and our hormones shift, it can have a big impact. In terms of symptoms 75-80 percent of us have to deal with hot flashes and night sweats, headaches and joint pains, being irritable and emotionally volatile, our concentration can decline; and 20-30% of us may experience severe symptoms. On top of that, there are some key changes to our metabolism, particularly blood sugar control.
04:18
So, what exactly happens to our bodies during menopause that makes blood sugar harder to manage? Well, it all comes down to how estrogen influences insulin and carbohydrate metabolism. When estrogen levels drop, a series of changes take place that affect how our bodies process and store glucose.
First, our pancreas—the organ that produces insulin—starts to slow down. Without estrogen’s support, the beta cells in the pancreas don’t release as much insulin, making it harder for our bodies to regulate blood sugar effectively.
Next, our muscles become less responsive to insulin. Normally, our muscles help absorb glucose from the bloodstream, keeping our blood sugar levels stable. But with lower estrogen levels, that process slows down, meaning more glucose lingers in the bloodstream instead of being used for energy.
At the same time, our liver starts producing more glucose than we need. This happens because insulin isn’t working as efficiently in the liver, so the body keeps making and releasing glucose—even when it’s not necessary. The liver also starts storing more fat, which can increase triglyceride levels and the production of VLDL cholesterol—a type of cholesterol linked to heart disease.
Then we have changes in fat storage. With lower estrogen, insulin struggles to regulate fat metabolism, leading to more fat breakdown but also larger fat cells that store more energy. These larger fat cells don’t just sit there—they actively release inflammatory chemicals that contribute to insulin resistance, making it even harder to keep blood sugar levels balanced. In addition, the type of fat we store changes. Instead of storing subcutaneous fat around our butt or hips, women often start seeing more belly fat, visceral fat that increases our risk of several health conditions, that’s because visceral fat releases inflammatory chemicals and further increases insulin resistance.
06:37
On top of this sarcopenia is common. Sarcopenia is an age related loss in lean muscle tissue. By the age of 60, you could have lost as much as 15% of your total muscle mass – that’s a huge amount; and during the menopause transition, this muscle loss is very obvious to many women. This muscle loss accelerates after menopause if we’re not actively working to maintain it. And since muscle is one of the main places where glucose is used, less muscle means less glucose being absorbed and more staying in your bloodstream. Less muscle mass further increases insulin resistance, not to mention affecting your strength and stamina.
Over time, these combined changes—lower insulin production, reduced glucose uptake, increased glucose production in the liver, increased fat storage, less muscle mass, and more inflammation—can lead to metabolic syndrome, a condition that increases the risk of type 2 diabetes, heart disease, and other metabolic issues. Basically metabolic syndrome produces a cluster of symptoms—high blood sugar, high blood pressure, altered cholesterol, and overweight or obesity.
But that’s not all. On top of the changes in metabolism and blood sugar control, we also have to contend with an increased rate of bone loss. Women lose an average of 2% bone mass during menopause, beginning 1–3 years before menopause and lasting 5–10 years, so overall that results in an average 10–12% decrease in bone mineral density in the spine and hip— that’s a lot and dramatically increases our risk of osteoporosis.
And just to add another level of complexity, during the menopause transition, our sleep quality can become compromised, which can further exacerbate blood sugar and metabolic balance.
Wow, that’s a lot isn’t it.
For many women it can feel like a bit of a vicious cycle, and like the odds are stacked up against us, and in many ways they are. These things are real, if you’ve noticed your body, your weight, your moods, or your health changing, you’re not going mad. It is true that our metabolism does slow down and can result in weight gain, even when you feel you haven’t changed anything. It is true that cravings may become more intense. It is true that energy levels may fluctuate significantly. It is true that concentration may be lacking and a complete brain fog that feels like a blanket over your head may take over some days. There are a vast array of symptoms that can arise and the key thing to know is that if you are in the menopause transition period, then it is likely due to the hormonal changes occurring in your body.
Of course, that part of it is out of our control, we can’t change the fact that our hormones change. It happens to every woman and we can’t escape it. What we do know is that making changes to our nutrition and lifestyle can help delay the development of symptoms, make them more bearable, and help make everyday life easier. And without a doubt, even though it may take a bit more work on our behalf, we can certainly change things in the opposite direction.
During this time of our life, we really need to be proactive with taking care of our health, and the reality is, we do need to make some changes to our lives to prioritize our health.
So that’s exactly what we’re going to talk about next, is what you can do about it, how you can support your metabolic health, particularly with nutrition, as nutrition is a very important factor throughout the stages of menopause.
11:34
Interestingly, a diabetes-friendly nutrition plan is the type of eating plan that will benefit most women during the menopause transitional phase, whether they have diabetes or not. And we also need to prioritize particular nutrients during this time to help support optimal metabolism.
First, let’s briefly cover things to avoid or eliminate from our nutrition plan and it really comes down to logic here with avoiding foods and drinks high in added sugar and refined carbohydrates – the white flour foods that worsen blood sugar and insulin resistance, like cakes, cookies, crackers, pastas, breads, all the packaged and processed foods that line the supermarket shelves. All the junky foods that we know are not the best choices for us. We want to focus on eating lots of fresh foods and avoid processed foods as much as possible.
If you’re a big coffee drinker, you might want to consider limiting your caffeine intake to no more than 3-4 cups a day of caffeinated drinks, as excessive caffeine consumption has been associated with calcium excretion and bone loss. And in postmenopause we may want to limit this even further to a couple of cups a day, just to ensure we’re not contributing to further bone loss.
Okay, many women don’t like hearing this next one, but there is great benefit if you stop drinking alcohol. During menopause, alcohol can worsen hormonal imbalances and amplify symptoms like hot flashes, sleep disturbances and mood swings. It also increases insulin resistance, making blood sugar harder to control, and contributes to weight gain, particularly around the abdomen. Plus, alcohol affects bone health, increasing the risk of osteoporosis by reducing calcium absorption. Since liver function slows with age, alcohol stays in the system longer, intensifying its effects so for us women, it can really do us a disservice. In contrast, cutting back—or eliminating alcohol—can help us women feel more balanced, improve sleep, and support overall metabolic and hormonal health during this transition.
In terms of nutrition, we need to ensure we are eating a high quality diet filled with a wide range of nutrient-rich foods. Focus on eating lots of vegetables for antioxidants like beta-carotene and vitamin K that support bone formation, as well as vitamins C and E and valuable polyphenols, which can help reduce oxidative stress and inflammation. Vitamin C also supports bone formation due to its role in collagen formation. Magnesium to improve energy metabolism and cellular function and support muscle function and reduce inflammation. Basically, lots of vitamins and minerals can help support our health.
Eating lots of vegetables provide a wide range of micronutrients that can help support our metabolism at this time, and they also happen to be the best type of carbohydrate to eat to maintain healthy blood sugar levels.
Vegetables also provide lots of fiber, and so do nuts and seeds. Fiber-rich foods can promote healthy intestinal flora, which can increase the level of biologically active estrogen in the body, slow the development of estrogen deficiency and reduce the menopausal symptoms we may experience. So ensure you’re getting at least 25 g a day of fiber.
Drink lots of water. Fluid intake is important in the transport of nutrients and oxygen around our body to help support cellular metabolism and the body’s natural balance, to help regulate the body’s heat balance, for detoxification, for a healthy gastrointestinal tract, and for healthy skin. During the menopause transition you may not feel as thirsty but you still need to drink lots of water, for all the reasons just mentioned.
B vitamins also play an important role in menopause. They play a fundamental role in the processing of carbohydrates and the functioning of the nervous system and in preventing cognitive dysfunction and cognitive decline. B vitamins are found in a variety of animal and plant-based foods. Meat, fish, eggs, and dairy. Leafy greens, legumes, nuts, and seeds and a variety of different vegetables, all help maintain optimal B vitamin levels.
Consume olive oil daily for its rich polyphenols and anti-inflammatory impacts. We did a whole podcast on the incredible benefits of olive oil in episode 14, so please listen to that.
To support better sleep, a regular eating schedule plays a key role in maintaining the circadian rhythm. Sleep is most affected by the timing and quality of dinner. It is recommended to have dinner at least 2 h before bedtime. Drinking a lot right before bedtime is not recommended.
We can also focus on supporting melatonin production with nutrition. Melatonin is a hormone that regulates sleep-wake cycles. During menopause, melatonin levels may decline, contributing to sleep disturbances, difficulty falling asleep, and nighttime awakenings.
Melatonin-rich food sources include eggs, fish, nuts, tart cherries, and strawberries. And we can also focus on vitamins and trace elements that participate as cofactors in melatonin synthesis, things like folic acid, vitamins B6 and B12, magnesium and zinc.
Another thing to focus on is getting adequate amounts of tryptophan. Tryptophan is a precursor of melatonin, and has a positive effect on sleep. Cheddar cheese and pumpkin seeds have a very high amount of tryptophan. Other foods rich in tryptophan are tuna and salmon, lamb, chicken breast and pork, tofu, eggs, sunflower seeds, almonds and peanuts.
What we see here again is we need a nutrient-rich diet to support our bodies on every single level. Quite literally, the foods we eat provide fuel for all our cells to function optimally and support hormonal balance as well.
19:55
In terms of our nutrition, there are some key nutrients we need to be particularly aware of.
We absolutely need to prioritize protein to help support the body to perform its functions and to sustain muscle mass. Protein is also essential for bone formation and maintenance, as it provides amino acids necessary for collagen synthesis that help build our bone matrix. We want to consume protein from a variety of sources, such as meats, poultry, fish, eggs, beans, legumes, nuts, seeds, and dairy products. Prioritizing protein at breakfast is also key, and we covered that in episode 69.
Now, two particular micronutrients we need to be aware of are calcium and vitamin D. It’s very important to have your vitamin D status checked, as low vitamin D levels make women more susceptible to osteoporosis. Getting vitamin D from sun exposure is the best option if you can, but if not, then supplementation is often necessary. In terms of foods, not many have vitamin D but you can include egg yolks, dairy products, offal, and foods enriched with vitamin D, which will all help improve your levels.
Then there’s calcium – we absolutely need to focus on getting our calcium intake daily and the recommended amount is 1000-1200mg calcium each day. It is best to achieve your calcium requirements through nutrition, rather than supplements, as calcium supplementation has been shown to increase cardiovascular risk. Dairy products contain the most easily absorbable calcium—parmesan cheese being a very high calcium source. For example, just eating one ounce or 28g of parmesan cheese per day contributes around 330 mg of calcium toward your daily calcium goal. Regular consumption of soft-boned fish (eaten with bones), such as canned sardines, pickled herring, anchovy and canned salmon, soy products like tofu and edamame, green leafy vegetables like spinach and bok choy, and tahini sesame paste are also good sources of calcium. Almonds and chia seeds are also good sources. We do have to put a little more thought into making sure we include lots of calcium-rich foods in our every day eating plan
We also need adequate vitamin D to help with calcium absorption, and protein and dietary fiber also help with calcium absorption.
So, while we surely haven’t covered everything there is to know, we didn’t cover exercise, sleep and stress in detail, as these are also areas we can focus on, but in terms of nutrition, there are a lot of things you can focus on here that are all going to help you regulate your blood sugar more effectively and to support better health during the menopause transition.
The most important thing? Being proactive. Making intentional choices with our food and self-care can help us feel stronger, more balanced, and more in control during this transition.
If you found this episode helpful, I’d love for you to share it with another woman who could benefit. And if you’re one of our members, please visit the library to find lots of additional resources for you alongside this podcast.
Until next time, take care of yourself.
Dr Jedha, over and out.
Subscribe to Type 2 Diabetes Talk on: Apple | Spotify | Amazon Music | Audible | YouTube | Podcast Index | Player FM | and more…

Ann Marie
I’m almost 20 years post menopause and diagnosed with DT2 about 9 years. I’ve also had ER positive breast cancer 5 years ago despite having low estrogen. My doctor is leery of increasing my estrogen levels due to the risk of breast cancer again so I’m in a do I or don’t I situation especially since the low estrogen is causing other problems in my body besides the affect on insulin resistance