Table of Contents[Hide][Show]
If you’ve ever found yourself constantly battling hunger with type 2 diabetes or prediabetes, you’re not alone. That insatiable craving, often referred to as “diabetes hunger,” can feel overwhelming, and at times, completely uncontrollable.
But there’s good news—by understanding what’s driving your hunger and taking targeted action, you can regain control, reduce cravings, and feel more satisfied after meals, warding off the hunger for good!
Let’s first explore why diabetes hunger happens before revealing one key step you can take to break the hunger cycle.
Why Does Diabetes Hunger Happen?
There are two factors involved in diabetes hunger:
- Blood sugar levels
- Altered hormone function
The Role of Blood Sugar in Driving Hunger
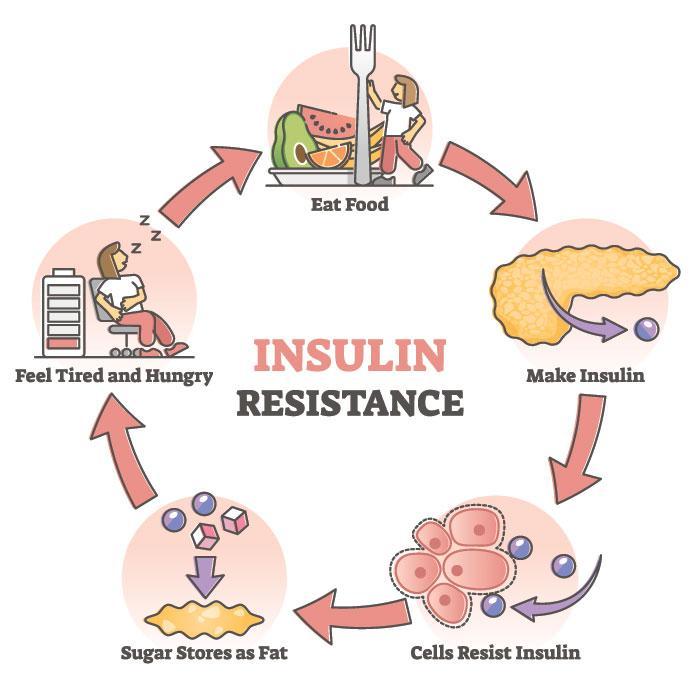
Hunger in diabetes often stems from imbalanced blood sugar levels. When your blood sugar is too high (hyperglycemia), it can disrupt how your body processes glucose.
Despite having an abundance of sugar in your bloodstream, your cells may not get enough energy, because in prediabetes and type 2 diabetes, energy can’t enter your cells efficiently—insulin resistance.
This leads to signals being sent to your brain that you’re hungry, even if you’ve just eaten.
In fact, high blood sugar disrupts how your body processes all nutrients, leading to an altered metabolism. When your metabolism becomes altered, various hormones throughout the body are affected.
It’s these hormones that manage hunger cues and signal our brain to react.
The Role of Hormones in Driving Hunger
Hormones like leptin, ghrelin, insulin, and cortisol play crucial roles in regulating hunger, appetite, and satiety (your feeling of fullness and satisfaction), especially for people with type 2 diabetes and prediabetes.
Here’s how these hormones function and how they relate to hunger in diabetes:
1. Leptin: The Satiety Hormone
Leptin, produced by fat cells, signals your brain when you’ve had enough to eat. It’s sometimes called the “satiety hormone” because its primary function is to reduce hunger and regulate energy balance.
People with diabetes and obesity often experience leptin resistance, where the brain becomes less responsive to leptin’s signals. This means that even with adequate leptin levels, your brain might still think you’re hungry.
Leptin resistance contributes to overeating and weight gain, perpetuating the cycle of insulin resistance and high blood sugar.

2. Ghrelin: The Hunger Hormone
Ghrelin, secreted by the stomach, stimulates appetite and increases food intake. It rises before meals and drops after eating.
Studies suggest that people with type 2 diabetes may have dysregulated ghrelin levels, leading to excessive hunger or cravings.
Elevated ghrelin can make it harder to resist overeating, particularly carbohydrate-rich foods.
3. Insulin: The Blood Sugar Regulator
Insulin is central to blood sugar control. After eating, insulin helps move glucose into cells for energy or storage. However, in type 2 diabetes and prediabetes, insulin resistance impairs this process, leaving glucose circulating in the bloodstream.
Insulin resistance often leads to excessive insulin production (hyperinsulinemia, HIGH insulin levels). High insulin levels can trigger hunger by signaling to the brain that more energy (food) is needed, even when blood sugar levels are already elevated.
4. Cortisol: The Stress Hormone
Cortisol, released during stress, can significantly influence hunger and blood sugar levels.
Chronic stress leads to prolonged cortisol elevation, which increases appetite and cravings, especially for sugary-rich foods. This response is partly a survival mechanism, as cortisol prepares the body for a “fight or flight” scenario by seeking quick energy sources.
Elevated cortisol can worsen insulin resistance, leading to higher blood sugar levels and increased hunger.
5. GLP-1: The Gut Hormone
Glucagon-like peptide-1 (GLP-1) is a hormone released by the gut after eating. Yes, it is the same hormone that Ozempic and Wegovy mimic, but it’s actually a natural hormone produced in your intestines.
GLP-1 promotes satiety and slows stomach emptying, helping to regulate blood sugar levels.
People with diabetes often have lower GLP-1 levels, contributing to increased hunger and faster gastric emptying. This can lead to overeating and blood sugar spikes.
While all of this sounds complex, the solution is quite simple.
Foods That Worsen Diabetes Hunger
Certain foods can intensify cravings and disrupt hormone balance. Avoiding or limiting these foods can prevent the rollercoaster of hunger signals and support better control of your appetite.
1. Refined Carbohydrates
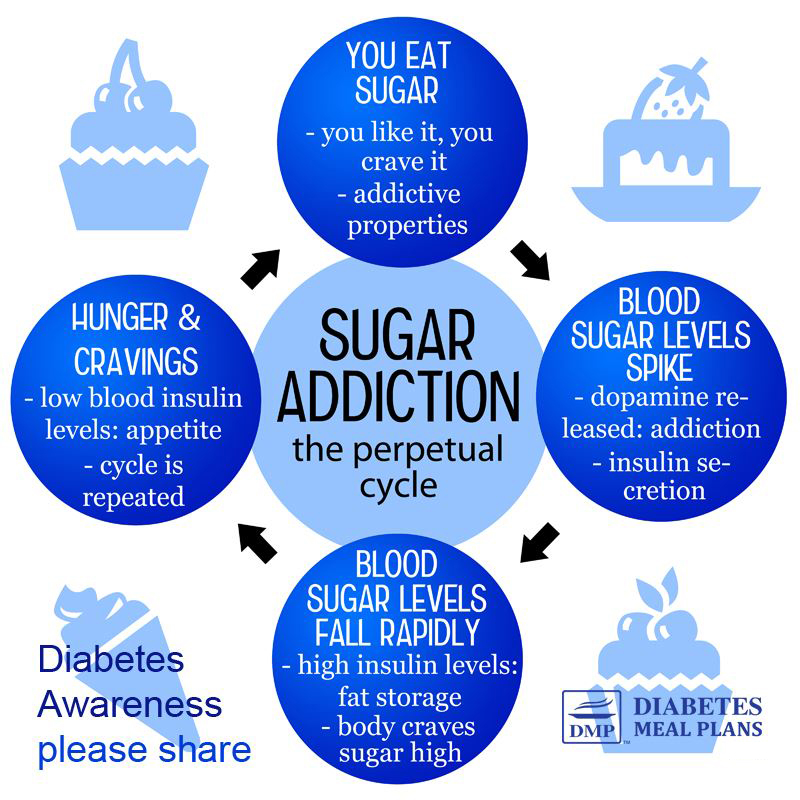
Foods like white bread, pastries, sugary cereals, and white rice cause rapid blood sugar spikes followed by steep crashes.
This triggers hunger hormones like ghrelin and increases insulin production, leaving you craving more food shortly after eating.
2. Sugary Foods and Drinks
Sweets, sodas, and even “healthy” options like fruit juices are high in sugar, which floods your bloodstream with glucose.
This overstimulates insulin release, driving intense hunger soon after consumption.
3. Low-Fat or Fat-Free Products
Many low-fat or fat-free foods are stripped of natural fats and replaced with sugar or refined starches to enhance flavor.
Without the satiety that fats provide, these foods can leave you feeling hungrier and less satisfied.
4. Processed Snack Foods
Chips, crackers, and packaged snacks are often high in refined carbs, unhealthy fats, and sodium.
These foods are engineered to be hyper-palatable, overstimulating your appetite and disrupting hunger-regulating hormones.
5. Alcohol
Alcohol not only lowers your inhibitions, making you more likely to overeat, but it also interferes with hunger hormones like leptin and ghrelin.
Drinking alcohol can increase cravings for calorie-dense, high-carb foods.
The One Key Step to Stop Diabetes Hunger: Prioritize Protein and Healthy Fats
To address hormonal imbalances, regulate blood sugar and break the hunger cycle, a single change can make a significant difference: prioritize protein and healthy fats in your meals.
How Protein Helps Reduce Hunger
Protein is the most satiating macronutrient. When you eat protein, it slows the absorption of glucose into your bloodstream, preventing blood sugar and insulin spikes and leads to more stable blood sugar levels.
Protein is also powerful ally in managing hunger because of its direct effects on the hormones that regulate appetite and blood sugar.
- Protein-rich meals can improve leptin sensitivity over time, allowing your brain to better recognize satiety signals.
- High-protein meals lead to a greater and longer-lasting reduction in hunger signals, helping you feel full for longer.
- Protein helps prevent sharp spikes in blood sugar and excessive insulin production, reducing hunger triggered by hyperinsulinemia.
- Protein is a GLP-1 boosting food, naturally stimulating the production of this hunger-regulating hormone, reducing the likelihood of overeating.
- During stressful times, consuming protein can help maintain blood sugar stability, reducing cortisol-induced cravings for sugary or high-fat foods.
Aim to include at least one protein source with every meal and snack.

How Eating Fat Helps Reduce Hunger
Healthy fats are another crucial component for managing diabetes hunger.
- Fats take longer to digest, which slows stomach emptying, suppressing ghrelin levels to prolong the feeling of fullness.
- Fats have a minimal impact on blood sugar, making them an excellent choice for stabilizing energy levels.
- Fats, especially omega-3 fatty acids, can improve leptin signaling, helping you feel full and satisfied.
- Healthy fats, particularly from sources like fatty fish and nuts, can reduce inflammation and counteract the stress-induced effects of cortisol. This can help stabilize appetite and support better blood sugar control.
Nutrient-Dense Foods to Ward Off Hunger
Combining protein with fats creates a synergistic effect, keeping hunger at bay for longer periods.
Let’s look at protein and fat-rich foods to include in your diet more often.
Examples of protein sources to include in your meals:
- Eggs
- Poultry (e.g., chicken, turkey)
- Seafood (e.g., salmon, tuna)
- Red meat
- Greek yogurt (unsweetened)
- Tofu, tempeh, or edamame
- Cottage cheese
Incorporate these healthy fats into your meals:
- Avocados
- Nuts and seeds (e.g., almonds, walnuts, chia seeds)
- Olive oil
- Fatty fish (e.g., salmon, mackerel)
- Coconut oil
- Full-fat dairy (if tolerated)
When paired with protein, fats create a powerful duo for curbing hunger and stabilizing blood sugar!
Meal Composition: The Power of Combining Protein, Fats, and Veggies
The best way to stop diabetes hunger is by building meals that combine protein, healthy fats, and non-starchy vegetables.
Non-starchy vegetables—like spinach, broccoli, zucchini, and peppers—are low in carbohydrates and high in fiber, which further enhances satiety and helps regulate blood sugar.
Here’s an example of how to structure a hunger-busting plate:
- Protein: Grilled chicken breast or baked salmon
- Healthy Fat: A drizzle of olive oil or a side of avocado or guacamole
- Vegetables: Steamed broccoli or mixed vegetables, roasted zucchini, or a mixed salad
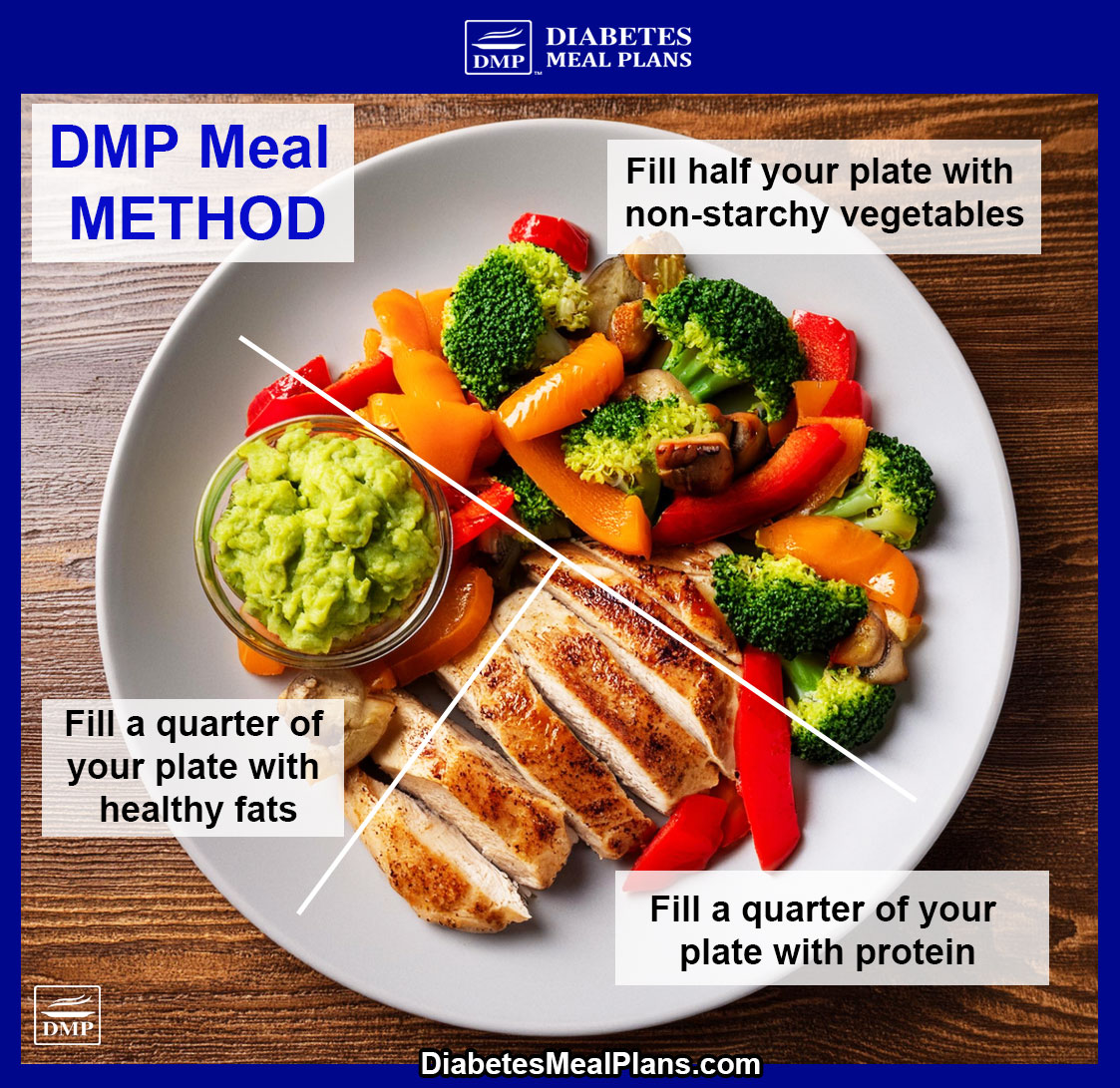
This simple formula ensures you’re eating balanced meals that keep hunger at bay for hours.
Of course, it doesn’t have to look like a plate of boring steamed vegetables and plain chicken. A healthy balanced plate can be a lot of different tasty meals.
Here’s some examples:
The key point is, by focusing on whole, nutrient-dense foods and minimizing these hunger-driving culprits, you can take control of your appetite and better manage your blood sugar and hormone balance.
Conclusion
Constant hunger doesn’t have to control your life. By prioritizing protein, healthy fats and lots of vegetables, you can stabilize your blood sugar levels, curb cravings, and feel more satisfied after meals.
Truly, start prioritizing protein and fat and everything will change for you!
These small but powerful changes can set you on a path to better health and give you the tools to stop diabetes hunger in its tracks.





George
Thank you. Forwarding to a friend in need, also
Dr Jedha
That’s wonderful George – thanks for supporting your friend!
Bill Braun
Terrific article and very helpful. Thank you.
Mary Hennicke
What about protein powder? Should I be using it?
Dr Jedha
Hi Mary, protein powder is an excellent addition to your eating routine as well. Here’s some of the best options, as it’s important to choose a quality one and many of them are not suitable.